J Korean Soc Radiol.
2015 Sep;73(3):164-167. 10.3348/jksr.2015.73.3.164.
Recurrent Breast Sparganosis: Clinical and Radiological Findings
- Affiliations
-
- 1Department of Radiology, Korea University Guro Hospital, Seoul, Korea. wokhee@korea.ac.kr
- 2Department of Radiology, Korea University Anam Hospital, Seoul, Korea.
- 3Department of Radiology, Korea University Ansan Hospital, Ansan, Korea.
- KMID: 2043606
- DOI: http://doi.org/10.3348/jksr.2015.73.3.164
Abstract
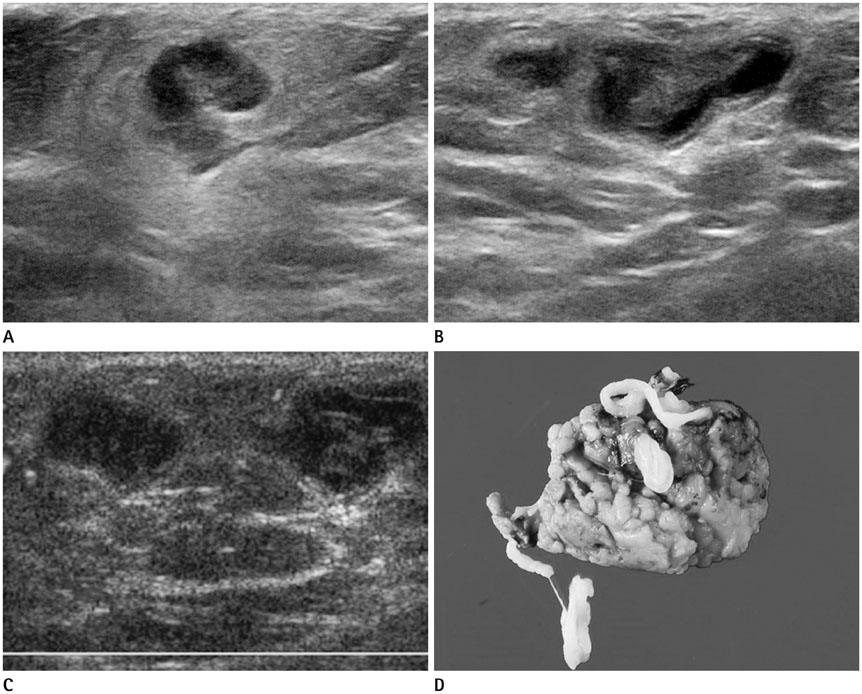
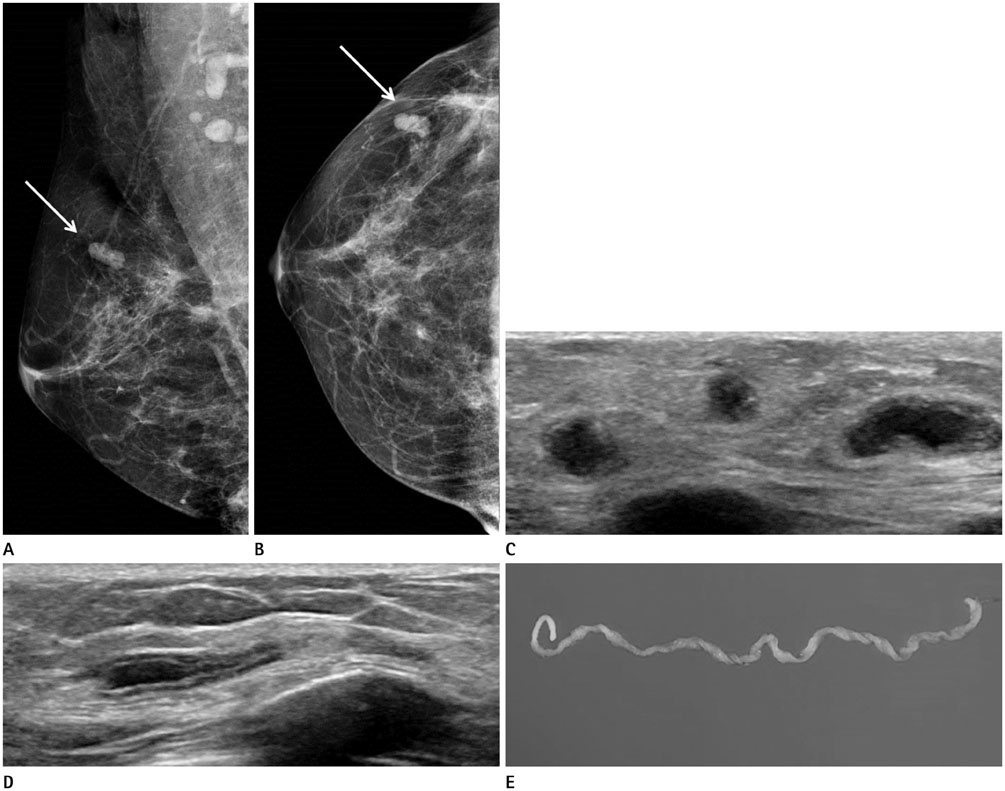
- We report a case of recurrent sparganosis of the breast within 6 months following surgical removal of worms from the breast. The patient was referred to our hospital with a palpable mass in the right breast. On admission, breast ultrasonography revealed a tortuous tubular hypoechoic lesion with indistinct margins within a surrounding hyperechoic area, which strongly suggested sparganosis. We performed surgical excision and confirmed sparganosis. After 6 months, the patient detected a new mass in her right breast and visited our hospital. Breast ultrasonography revealed similar features in a different area of the same breast. We confirmed recurrent sparganosis surgically.
Figure
Reference
-
1. Cho SY, Bae JH, Seo BS. Some aspects of human sparganosis in Korea. Korean J Parasitol. 1975; 13:60–77.2. Yoon HS, Jeon BJ, Park BY. Multiple sparganosis in an immunosuppressed patient. Arch Plast Surg. 2013; 40:479–481.3. Koo M, Kim JH, Kim JS, Lee JE, Nam SJ, Yang JH. Cases and literature review of breast sparganosis. World J Surg. 2011; 35:573–579.4. Moon HG, Jung EJ, Park ST. Breast sparganosis presenting as a breast mass with vague migrating pain. J Am Coll Surg. 2008; 207:292.5. Park HJ, Park NH, Lee EJ, Park CS, Lee SM, Park SI. Ultrasonographic findings of subcutaneous and muscular sparganosis. J Korean Soc Radiol. 2009; 61:183–187.6. Kim JW, Hwang MS. Sparganosis of the breast that mimicked metastasis: a case report. J Korean Soc Ultrasound Med. 2011; 30:59–62.7. Choi SJ, Park SH, Kim MJ, Jung M, Ko BH. Sparganosis of the breast and lower extremities: sonographic appearance. J Clin Ultrasound. 2014; 42:436–438.8. Oh YJ, Kim MJ, Cho JH, Cha CW, Kim DH, Oh MJ, et al. A case of pulmonary sparganosis in a patient with a history of recurrent sparganum infections. Tuberc Respir Dis. 2009; 67:229–233.9. Lee YI, Seo M, Park HW. Recurred sparganosis 1 year after surgical removal of a sparganum in a Korean woman. Korean J Parasitol. 2014; 52:75–78.10. Kubota T, Itoh M. Sparganosis associated with orbital myositis. Jpn J Ophthalmol. 2007; 51:311–312.