J Korean Soc Radiol.
2014 Apr;70(4):283-289. 10.3348/jksr.2014.70.4.283.
In Vivo Location of the Vermiform Appendix in Multidetector CT
- Affiliations
-
- 1Department of Radiology, Uijeongbu St. Mary's Hospital, College of Medicine, The Catholic University of Korea, Uijeongbu, Korea.
- 2Department of Radiology, Seoul St. Mary's Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea. jybyun@catholic.ac.kr
- KMID: 2041939
- DOI: http://doi.org/10.3348/jksr.2014.70.4.283
Abstract
- PURPOSE
To provide a more detailed classification system regarding the position of the vermiform appendix within the right lower quadrant, as seen on multidetector computed tomography (MDCT) and to investigate the relative differences in frequency of appendiceal position according to patient gender and the pathologic state of appendix.
MATERIALS AND METHODS
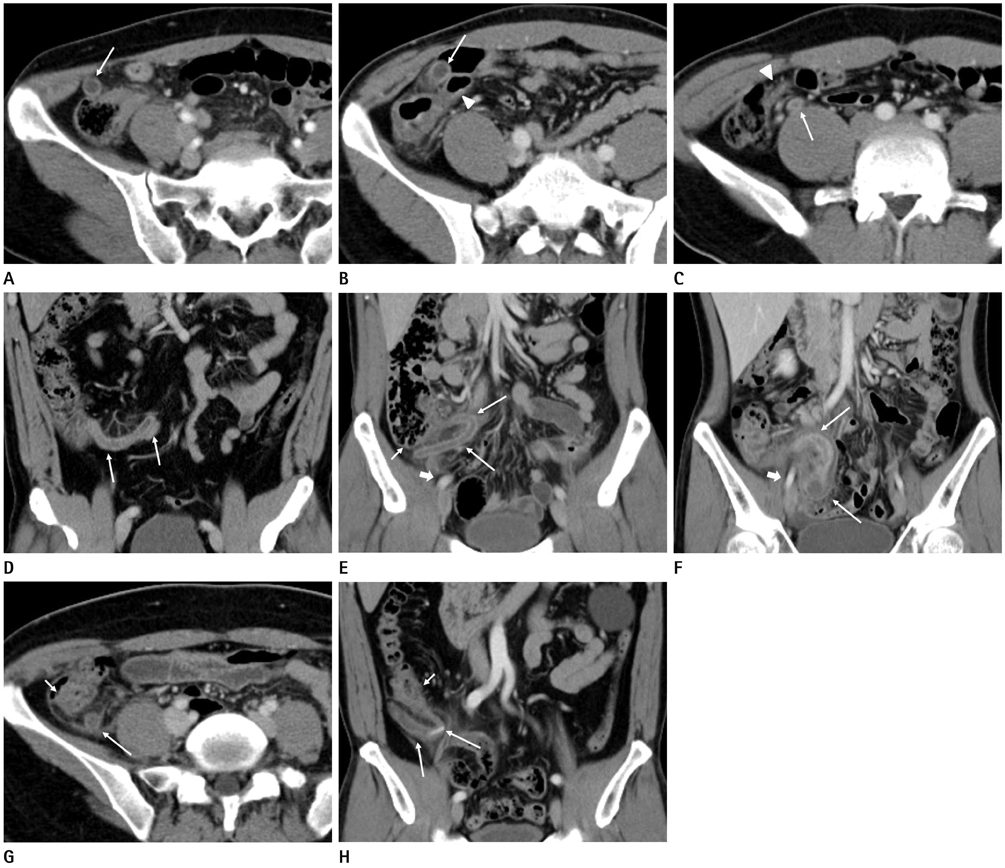
Between January 2008 and December 2010, 1157 patients were included in our final analysis: 542 patients with preoperative MDCT and subsequent appendectomy and 615 patients with visible appendix seen on MDCT performed as part of a health checkup. We classified the appendix according to its position relative to the cecum, the terminal ileum, and the external iliac vessels: type 1: antececal; type 2: preileal; type 3: postileal; type 4: subileal; type 5: subcecal; type 6: deep pelvic; type 7: retrocecal; and type 8: paracecal.
RESULTS
The relative incidence of various positions of the appendix found in all of our study patients was: type 1: 3.5%; type 2: 1.7%; type 3: 9.0%; type 4: 12.9%; type 5: 42.3%; type 6: 16.2%; type 7: 10.9%; and type 8: 3.0%. According to patient gender, type 1 (male: 3.7% vs. female: 3.3%), type 3 (8.6% vs. 9.8%), type 4 (14.3% vs. 9.8%), type 5 (47.5% vs. 32.7%), type 7 (9.2% vs. 14.4%), and type 8 (3.4% vs. 2.2%) positions showed a statistically significant male predominance. In terms of the inflamed state, type 2 preileal (normal: 0.8% vs. inflamed: 2.8%), type 3 (10.2% vs. 7.6%), type 4 (14.0% vs. 11.6%), and type 5 (14.1% vs. 18.5%) positions showed a statistically significant difference.
CONCLUSION
Contrary to the common assumption that the retrocecal appendix is the most common position, the in vivo appendix is seen more often on MDCT in the subcecal and deep pelvic positions. The relative frequency of various positions of the appendix can also differ according to patient gender and the pathologic state.
MeSH Terms
Figure
Reference
-
1. Paulson EK, Harris JP, Jaffe TA, Haugan PA, Nelson RC. Acute appendicitis: added diagnostic value of coronal reformations from isotropic voxels at multi-detector row CT. Radiology. 2005; 235:879–885.2. Moneer MM. Avoiding muscle cutting while extending McBurney's incision: a new surgical concept. Surg Today. 1998; 28:235–239.3. Chan WT, Cheng NHY, Cheng KC, Cheung KKT, Cheung MH, Ho KKH, et al. Does appendix position affect the clinical outcome of acute appendicitis? Ann Coll Surg Hong Kong. 2002; 6:109–112.4. Wakeley CP. The Position of the Vermiform Appendix as Ascertained by an Analysis of 10,000 Cases. J Anat. 1933; 67(Pt 2):277–283.5. Maa J, Kirwood KS. The appendix. In : Sabiston DC, Townsend CM, editors. Textbook of Surgery: The Biological Basis of Modern Surgical Practice. 19th ed. Philadelphia: Elsevier Saunders;2012. p. 1279–1293.6. Maisel H. The position of the human vermiform appendix in fetal and adult age groups. Anat Rec. 1960; 136:385–391.7. Picken G, Ellis H, Dixon AK. The normal vermiform appendix at computed tomography: visualization and anatomical location. Clin Anat. 1993; 6:9–14.8. Baldisserotto M, Marchiori E. Accuracy of noncompressive sonography of children with appendicitis according to the potential positions of the appendix. AJR Am J Roentgenol. 2000; 175:1387–1392.9. Ahmed I, Asgeirsson KS, Beckingham IJ, Lobo DN. The position of the vermiform appendix at laparoscopy. Surg Radiol Anat. 2007; 29:165–168.10. Oh KJ, Cho JS, Shin KS, Kim HY, Lim SK, Ohm JY, et al. Normal appendix in adults: MDCT findings about the location, thickness and the presence or absence of intraluminal gas. J Korean Radiol Soc. 2006; 55:373–379.11. Prystowsky JB, Pugh CM, Nagle AP. Current problems in surgery. Appendicitis. Curr Probl Surg. 2005; 42:688–674.12. Rybkin AV, Thoeni RF. Current concepts in imaging of appendicitis. Radiol Clin North Am. 2007; 45:411–422.13. Chalazonitis AN, Tzovara I, Sammouti E, Ptohis N, Sotiropoulou E, Protoppapa E, et al. CT in appendicitis. Diagn Interv Radiol. 2008; 14:19–25.14. Schumpelick V, Dreuw B, Ophoff K, Prescher A. Appendix and cecum. Embryology, anatomy, and surgical applications. Surg Clin North Am. 2000; 80:295–318.15. Ramsden WH, Mannion RA, Simpkins KC, deDombal FT. Is the appendix where you think it is--and if not does it matter? Clin Radiol. 1993; 47:100–103.16. Malas MA, Gökçimen A, Sulak O. Growing of caecum and vermiform appendix during the fetal period. Fetal Diagn Ther. 2001; 16:173–177.17. Moore KL, Dalley AF II. The pelvis and perineum. In : Moore KL, Dalley AF, editors. Clinically oriented anatomy. 5th ed. Philadelphia: Lippincott Williams & Wilkins;2006. p. 357–471.18. Jorge A, Ferreira JR, Pacheco YG. Development of the vermiform appendix in children from different age ranges. Braz J Morphol Sci. 2009; 26:68–76.19. O'Connor CE, Reed WP. In vivo location of the human vermiform appendix. Clin Anat. 1994; 7:139–142.20. Clegg-Lamptey JN, Armah H, Naaeder SB, Adu-Aryee NA. Position and susceptibility to inflammation of vermiform appendix in Accra, Ghana. East Afr Med J. 2006; 83:670–673.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Preoperative Diagnosis of Diverticulitis of the Vermiform Appendix by Ultrasonography
- CT Features of Appendiceal Mucocele
- A Case Report of Intussusception of the Vermiform Appendix with Adenocarcinoma
- Umbilical Cord Hernia Containing Vermiform Appendix Adherent to the Sac
- Appendiceal Diverticulosis Presented with Cecal Dicerticulitis