J Korean Soc Spine Surg.
2006 Mar;13(1):1-9. 10.4184/jkss.2006.13.1.1.
A Minimum Follow-up Study of 10 years After Pedicle Screw Fixation and Fusion for Degenerative Lumbar Diseases
- Affiliations
-
- 1Department of Orthopaedic Surgery, Soonchunhyang University College of Medicine, Spine center Seoul Hospital, Seoul, Korea. schsbj@hosp.sch.ac.kr
- 2Department of Orthopaedic Surgery, Soonchunhyang University College of Medicine, Gumi Hospital, Gumi, Korea.
- KMID: 2040774
- DOI: http://doi.org/10.4184/jkss.2006.13.1.1
Abstract
-
STUDY DESIGN: A retrospective study was conducted. OBJECTIVES: To evaluate the long-term clinical results and radiological changes of lumbar spinal fusions with pedicle screw fixation for degenerative lumbar disease.
SUMMARY OF LITERATURE REVIEW: Pedicle screw fixation of the lumbar spine is a widely used procedure, but there is little longterm follow-up information on the results of the technique.
MATERIALS AND METHODS
Patients, who underwent surgery for degenerative lumbar diseases, from May 1988 through December 1994, were included. Those patients who received surgery for tumors, infections, traumas, and deformities were excluded, as were those who received long-level fusions . The clinical results were evaluated with Kim's criteria. Radiologically, changes in lumbar lordosis and disc height were measured, and calcification in the disc spaces was evaluated.
RESULTS
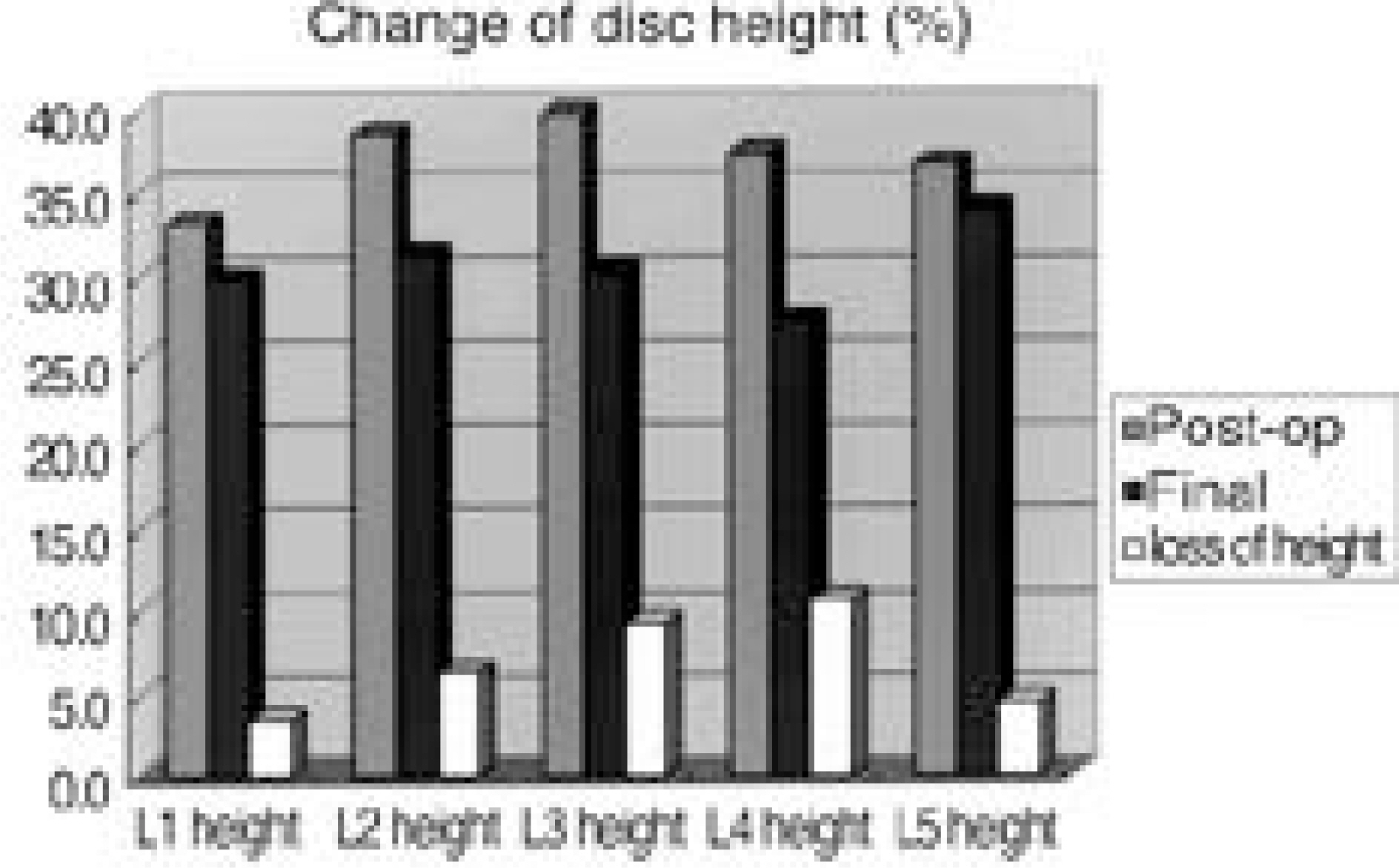
One hundred-thirty-six patients matched the study criteria. Of these, 13 had died, and there were 123 available for the study. Clinical follow-up was completed in 58 patients. There were 36 women and 22 men. The average age at the time of surgery was 52.7 years. The average follow-up was 148 months. Forty-four patients had satisfactory results at the final follow-up. Repeat surgery was necessary in 7 patients: 6 of them on a single segment and 4 with a posterior lumbar interbody fusion. A final radiologic analysis was completed in 44 patients. Lumbar lordosis was reduced from 43 degrees to 33 degrees. The lordotic angle of the fusion segments was reduced from 22 degrees to 13 degrees. The relative heights of the discs were markedly reduced at L3-4 and L4-5, from 40% to 30% and from 37% to 27%, respectively. Calcification of the disc space was observed in 37 segments out of a total of 58 that were treated with posterolateral fusions.
CONCLUSION
The clinically satisfactory result rate was similar to that of the 5-year follow-up reported in a previous study by the author. Repeat operations were necessary if disc herniation or stenosis developed in the adjacent vertebral segments. Patients who were treated with a single-level PLIF demonstrated a higher repeat operation rate. Lordotic angles and disc space heights were reduced significantly during the follow-up period. Many disc spaces (64%) involved in posterolateral fusions had calcific deposits, which meant that spontaneous disc space fusion would occur over time, even though the disc space was not fused at the time of surgery.
MeSH Terms
Figure
Reference
-
1). Krag MH, Beynnon BD, Pope MH, Frymoyer JW, Haugh LD, Weaver DL. An internal fixator for posterior application to short segments of the thoracic, lumbar or lumbosacral spine. Clin Orthop. 1986; 203:75–98.2). Roy-Camille R, Saillant G, Mazel C. Internal fixation of the lumbar spine with pedicle screw plating. Clin Orthop. 1986; 203:7–17.
Article3). Kim NH, Kim DJ. Anterior interbody fusion for spondylolisthesis. Orthopedics. 1991; 14:1069–1076.
Article4). Glaser J, Stanley M, Sayre H, Woody J, Found E, Spratt K. A 10-year follow-up evaluation of lumbar spine fusion with pedicle screw fixation. Spine. 2003; 28:1390–1395.
Article5). Shin BJ, Lee JJ. Results of decompression and internal fixation for spinal stenosis more than 5 year follow-up. J Kor Spine Surg. 1998; 2:272–277.6). Lehmann TR, Spratt KF, Tozzi JE, et al. Long-term follow-up of lower lumbar fusion patients. Spine. 1987; 12:97–104.
Article7). Hambly MF, Wiltse LL, Raghavan N, Schneiderman G, Koenig C. The transition zone above a lumbosacral fusion. Spine. 1998; 15:1785–1792.
Article8). Chung SM. Brief notes. Methods for locating the “ Missing patients” in long-term follow-up studies. J Bone Joint Surg. 1971; 53:1448–1451.9). Christensen FB, Hansen ES, Laursen M, Thomsen K, Bunger CE. Long-term functional outcome of pedicle screw instrumentation as a support for posterolateral fusion. Spine. 2002; 27:1269–1277.10). Kuroki H, Tajima N, Kubo S. Clinical results of posterolateral fusion for degenerative lumbar spinal diseases: a follow-up study of more than 10 years. J Orthop Sci. 2002; 7:317–324.
Article11). Brantigan JW, Neidre A, Toohey JS. The lumbar I/F cage for posterior lumbar interbody fusion with the variable screw placement system: 10-year results of a Food and Drug Administration clinical trial. Spine J. 2004; 4:681–688.
Article12). Fischgrund JS, Mackay M, Herkowitz HN, Brower R, Montgomery DM, Kurz LT. 1997 Volvo Award winner in clinical studies. Degenerative lumbar spondylolisthesis with spinal stenosis: a prospective, randomized study comparing decompressive laminectomy and arthrodesis with and without spinal instrumentation. Spine. 1997; 22:2807–2812.13). Thomsen K, Christensen FB, Eiskjaer SP, Hansen ES, Fruensgaard S, Bunger CE. 1997 Volvo Award winner in clinical studies. The effect of pedicle screw instrumentation on functional outcome and fusion rates in posterolateral lumbar spinal fusion: a prospective, randomized clinical study. Spine. 1997; 22:2813–22.14). Frymoyer JW, Hanley E, Howe J, Kuhlmann D, Matteri R. Disc excision and spine fusion in the management of lumbar disc disease; A minimum ten-year follow-up. Spine. 1978; 3:1–6.15). Rahm MD, Hall BB. Adjacent-Segment Degeneration After Lumbar Fusion with Instrumentation: A Retrospective Study. J Spinal Disord. 1996; 9:392–400.16). Kumar MN, Jacquot F, Hall H. Long-term follow-up of functional outcomes and radiographic changes at adjacent levels following lumbar spine fusion for degenerative disc disease. Eur Spine J. 2001; 10:309–313.
Article17). Frymoyer JW, Hanley EN Jr., Howe J, Kuhlmann D, Matteri RE. A comparison of radiographic findings in fusion and nonfusion patients ten or more years following lumbar disc surgery. Spine. 1979; 4:435–440.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Comparison between Posterolateral Fusion with Pedicle Screw Fixation and Anterior Interbody Fusion with Pedicle Screw Fixation in Spondylolytic Spondylolisthesis of the Lumbar Spine
- Unilateral Pedicle Screw Fixation in Degenerative Lumbar Spinal Stenosis
- Cotrel - Dubousset Pedicle Screw Fixation After Posterior Decompression of Lumbar Spinal Stenosis
- The Comparison of Changes in the Dimensions of the Intervertebral Disc and Neural Foramen between Anterior Lumbar Interbody Fusion and Posterolateral Fusion in the Lumbar Spine
- Efficacy of Posterior Lumbar Interbody Fusion using PEEK Cage and Pedicle Screw Stabilization in Degenerative Lumbar Spinal Disorders: Minimum 3 Years Follow up Results