J Korean Fract Soc.
2014 Oct;27(4):301-307. 10.12671/jkfs.2014.27.4.301.
The Efficacy of Preserved Posterior Cortex in the Treatment of Infected Nonunion of the Tibia
- Affiliations
-
- 1Department of Orthopedic Surgery, The Catholic University of Korea, Buchon St. Mary's Hospital, Bucheon, Korea. osleejy@catholic.ac.kr
- KMID: 2015486
- DOI: http://doi.org/10.12671/jkfs.2014.27.4.301
Abstract
- PURPOSE
We studied the efficacy of preserved posterior cortex connecting to adjacent muscle or periosteum during wide debridement in the treatment of infected nonunion of the tibia.
MATERIALS AND METHODS
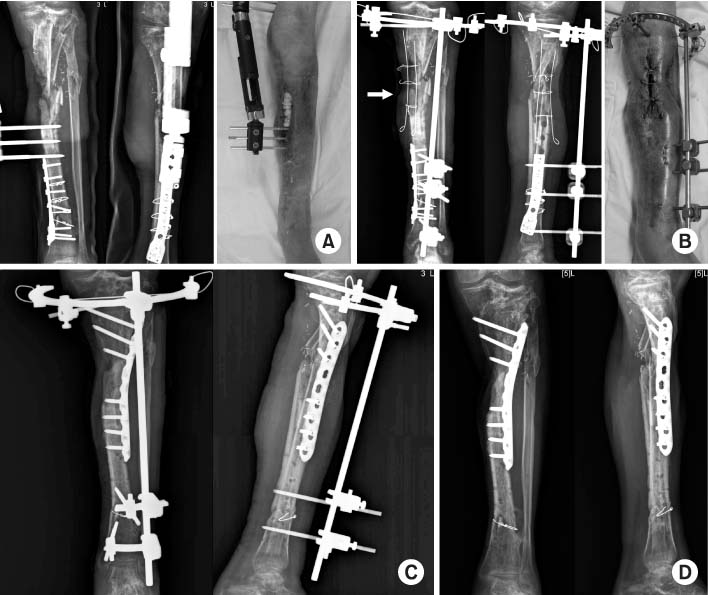
From January 2001 to May 2011, 12 cases of infected nonunion of the tibia with segmental defect larger than 4 cm after wide debridement were selected. The selected cases were categorized according to two groups; group 1 with preserved posterior cortex in the segmental defect site - six cases, group 2 without posterior cortex - six cases. The results were compared by assessing the size of bone defect, the interval between wide debridement and bone reconstruction, bony union time, complications, and clinical results.
RESULTS
The mean length of bone defect of group 1 was 7.6 cm (range 4.3-11.0 cm) and that of group 2 was 6.4 cm (range 4.0-12.0 cm). The interval between wide debridement and bone reconstruction was 10.0 weeks (range 5-18 weeks) for group 1, and 12.1 weeks (range 0-24 weeks) for group 2. The time for bony union of group 1 was 6.2 months (range 5-7 months), and that of group 2 was 10.8 months (range 7-18 months). In group 2, there were two cases of fatigue fracture and two cases of docking site nonunion after distraction osteogenesis.
CONCLUSION
The preserved posterior cortex after wide debridement of infected nonunion of the tibia helps bony union and reduces the treatment period.
Keyword
Figure
Reference
-
1. Kim HM, Kim YS, Chu IT, Choi MG, Cho YG. Free vascularized fibular graft for the treatment of the large bone defect. J Korean Orthop Assoc. 1995; 30:1224–1231.
Article2. Gustilo RB, Anderson JT. Prevention of infection in the treatment of one thousand and twenty-five open fractures of long bones: retrospective and prospective analyses. J Bone Joint Surg Am. 1976; 58:453–458.
Article3. Patzakis MJ, Abdollahi K, Sherman R, Holtom PD, Wilkins J. Treatment of chronic osteomyelitis with muscle flaps. Orthop Clin North Am. 1993; 24:505–509.
Article4. Patzakis MJ, Wilkins J. Factors influencing infection rate in open fracture wounds. Clin Orthop Relat Res. 1989; (243):36–40.
Article5. Damholt VV. Treatment of chronic osteomyelitis; a prospective study of 55 cases treated with radical surgery and primary wound closure. Acta Orthop Scand. 1982; 53:715–720.
Article6. Patzakis MJ, Zalavras CG. Chronic posttraumatic osteomyelitis and infected nonunion of the tibia: current management concepts. J Am Acad Orthop Surg. 2005; 13:417–427.
Article7. Weiland AJ, Daniel RK. Microvascular anastomoses for bone grafts in the treatment of massive defects in bone. J Bone Joint Surg Am. 1979; 61:98–104.
Article8. Vail TP, Urbaniak JR. Donor-site morbidity with use of vascularized autogenous fibular grafts. J Bone Joint Surg Am. 1996; 78:204–211.
Article9. Green SA. Skeletal defects. A comparison of bone grafting and bone transport for segmental skeletal defects. Clin Orthop Relat Res. 1994; (301):111–117.
Article10. DeCoster TA, Gehlert RJ, Mikola EA, Pirela-Cruz MA. Management of posttraumatic segmental bone defects. J Am Acad Orthop Surg. 2004; 12:28–38.
Article11. Christian EP, Bosse MJ, Robb G. Reconstruction of large diaphyseal defects, without free fibular transfer, in Grade-IIIB tibial fractures. J Bone Joint Surg Am. 1989; 71:994–1004.
Article12. Reckling FW, Waters CH 3rd. Treatment of non-unions of fractures of the tibial diaphysis by posterolateral cortical cancellous bone-grafting. J Bone Joint Surg Am. 1980; 62:936–941.
Article13. Simpson JM, Ebraheim NA, An HS, Jackson WT. Posterolateral bone graft of the tibia. Clin Orthop Relat Res. 1990; (251):200–206.
Article14. Song JM, Kim JI, Park JS, et al. A clinical study of free vascularized osteocutaneous fibular transplantation in infected nonunion of tibia. J Korean Soc Microsurg. 2000; 9:27–36.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Papineau Technique for Infected Nonunion of Tibia: Clinical Analysis
- Relationship of Tibial Nonunion with Fibular Nonunion in the Tibio-fibular Shaft Fracture
- The Antibiotic Cement Coated Nail and Masquelet Technique for the Treatment of Infected Nonunion of Tibia with Bone Defect and Varus Deformity
- Treatment of Nonunion of Tibia with Extracorporeal Shock Wave Therapy: A Case Report
- Radical Necrotic Bone Resection and Ilizarov Technique for Infected Nonunion of the Tibia