Compliance with Positive Airway Pressure Treatment for Obstructive Sleep Apnea
- Affiliations
-
- 1Department of Otolaryngology, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea. yschung@amc.seoul.kr
- 2Department of Otolaryngology, National Police Hospital, Seoul, Korea.
- KMID: 2007191
- DOI: http://doi.org/10.3342/ceo.2009.2.2.90
Abstract
OBJECTIVES
Positive airway pressure (PAP) is considered a standard treatment for moderate-to-severe obstructive sleep apnea (OSA) patients. However, compliance with PAP treatment is suboptimal because of several types of discomfort experienced by patients. This study investigated compliance with PAP therapy, and affecting factors for such compliance, in OSA patients.
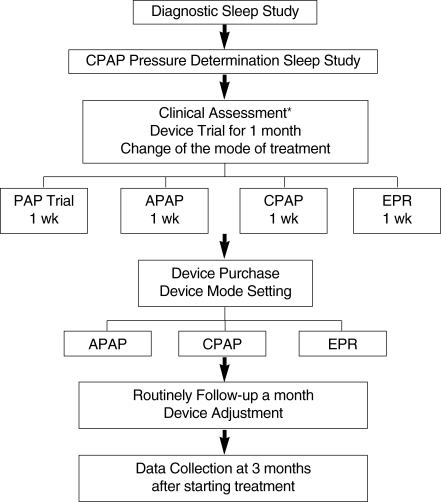
METHODS
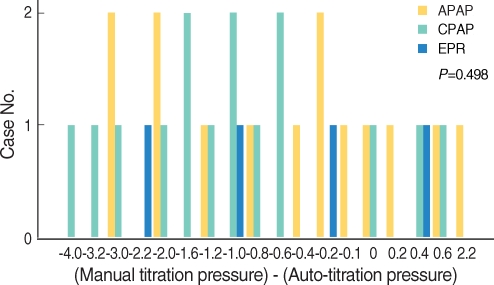
We performed a survey on 69 patients who engaged in PAP therapy between December 2006 and November 2007. After diagnostic polysomnography and manual titration, patients trialed PAP using the ResMed instrument and explored autoadjusting PAP (APAP), continuous PAP (CPAP), and flexible PAP (using expiratory pressure relief [EPR]) at least once every week for 1 month. Compliance measures were mean daily use (hr), percentage of days on which PAP was used, and percentage of days on which PAP was used for >4 hr. Data were obtained at night using the software Autoscan version 5.7(R) of the ResMed Inc. We obtained data on anthropometric (age, BMI, neck circumflex, Epworth sleepiness scale, Pittsburgh Sleep Quality Index, hypertension, alcohol intake), polysomnographic data (severity of apnea-hypopnea index [AHI], proportion of nonsupine sleep time, position dependence of sleep), PAP mode and AHI during PAP use for affecting factors.
RESULTS
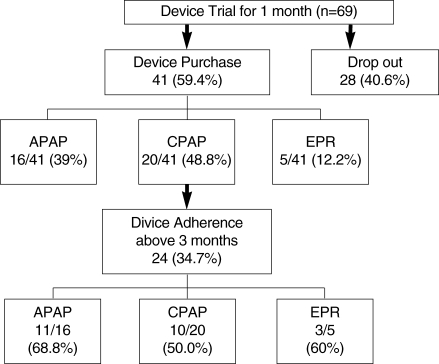
After 1 month, 41 of the 69 patients (59.4%) were pleased with PAP therapy and purchased instruments. Twenty-four patients (34.7%) used PAP for more than 3 months. The percentage of days on which PAP was used was statistically higher in patients with hypertension than in normotensive patients (P=0.003). There were negative correlations 1) between nonsupine position sleep time and percentage of days on which PAP was used (r=-0.424, P=0.039), and 2) between the AHI during PAP use and the percentage of days on which PAP was used for >4 hr (r=-0.443, P=0.030). There were no statistical differences between AHI, BMI, PAP pressure, or other measured parameters, on the one hand, and compliance, on the other.
CONCLUSION
The affecting factors for PAP use were hypertension history, sleep posture (shorter nonsupine sleep time), and lower AHI during PAP use.
Keyword
MeSH Terms
Figure
Cited by 7 articles
-
Predictors of Adherence with Positive Airway Pressure Treatment in Patients with Obstructive Sleep Apnea in Korean
Jin Myung Kim, Min Jae Kim, Sung Hee Bae, Chan Hum Park, Dong-Kyu Kim
J Rhinol. 2015;22(2):89-95. doi: 10.18787/jr.2015.22.2.89.Initial Adherence to Autotitrating Positive Airway Pressure Therapy: Influence of Upper Airway Narrowing
Yoon Kyoung So, Hun-Jong Dhong, Hyo Yeol Kim, Seung-Kyu Chung, Jeon-Yeob Jang
Clin Exp Otorhinolaryngol. 2009;2(4):181-185. doi: 10.3342/ceo.2009.2.4.181.Optimal Continuous Positive Airway Pressure Level in Korean Patients with Obstructive Sleep Apnea Syndrome
Ji Ho Choi, Eun Joong Kim, Kang Woo Kim, June Choi, Soon Young Kwon, Heung Man Lee, Tae Hoon Kim, Sang Hag Lee, Chol Shin, Seung Hoon Lee
Clin Exp Otorhinolaryngol. 2010;3(4):207-211. doi: 10.3342/ceo.2010.3.4.207.Maxillomandibular Advancement and Upper Airway Stimulation: Extrapharyngeal Surgery for Obstructive Sleep Apnea
Myeong Sang Yu, Badr Ibrahim, Robert Wayne Riley, Stanley Yung-Chuan Liu
Clin Exp Otorhinolaryngol. 2020;13(3):225-233. doi: 10.21053/ceo.2020.00360.Adherence to Positive Airway Pressure therapy as Severity of Adult Obstructive Sleep Apnea
Seongbin Park, Min Young Seo, Min Kyu Lee, Mun Soo Han, Jun Yoo, Sun Jin Hwang, Seung Hoon Lee
Korean J Otorhinolaryngol-Head Neck Surg. 2022;65(3):150-156. doi: 10.3342/kjorl-hns.2021.00556.Compliance After Re-Prescription for Positive Airway Pressure in Obstructive Sleep Apnea Patients Who Failed Positive Airway Pressure Therapy
Jeonghyun Lee, JunYeong Jeong, Jaeha Lee, Jae Yong Lee, Ji Ho Choi
J Rhinol. 2022;29(3):148-154. doi: 10.18787/jr.2022.00417.Trends in Palate Surgery for Obstructive Sleep Apnea in Korea Over the Past 12 Years
Jae Hoon Cho, Ji Ho Choi
J Rhinol. 2023;30(3):129-134. doi: 10.18787/jr.2023.00040.
Reference
-
1. Loube DI, Gay PC, Strohl KP, Pack AI, White DP, Collop NA. Indications for positive airway pressure treatment for adult obstructive sleep apnea patients: a consensus statement. Chest. 1999; 3. 115(3):863–866. PMID: 10084504.2. McArdle N, Devereux G, Heidarnejad H, Engleman HM, Mackay TW, Douglas NJ. Long-term use of CPAP therapy for sleep apnea/hypopnea syndrome. Am J Respir Crit Care Med. 1999; 4. 159(4 Pt 1):1108–1114. PMID: 10194153.
Article3. Engleman HM, Wild MR. Improving CPAP use by patients with the sleep apnea/hypopnea syndrome. Sleep Med Rev. 2003; 2. 7(1):81–99. PMID: 12586532.4. Kakkar RK, Berry RB. Positive airway pressure treatment for obstructive sleep apnea. Chest. 2007; 9. 132(3):1057–1072. PMID: 17873201.
Article5. Aloia MS, Stanchina M, Arnedt JT, Malhotra A, Millman RP. Treatment adherence and outcomes in flexible vs standard continuous positive airway pressure therapy. Chest. 2005; 6. 127(6):2085–2093. PMID: 15947324.
Article6. Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL Jr, et al. The seventh report of the Joint National Committee on prevention, detection, evaluation, and treatment of high blood pressure: the JNC 7 report. JAMA. 2003; 5. 21. 289(19):2560–2572. PMID: 12748199.
Article7. Pepin JL, Krieger J, Rodenstein D, Cornette A, Sforza E, Delguste P, et al. Effective compliance during the first 3 months of continuous positive airway pressure: a European prospective study of 121 patients. Am J Respir Crit Care Med. 1999; 10. 160(4):1124–1129. PMID: 10508797.8. Galetke W, Anduleit N, Richter K, Stieglitz S, Randerath WJ. Comparison of automatic and continuous positive airway pressure in a night-by-night analysis: a randomized, crossover study. Respiration. 2008; 75(2):163–169. PMID: 17148931.
Article9. Marshall NS, Neill AM, Campbell AJ. Randomised trial of compliance with flexible (C-Flex) and standard continuous positive airway pressure for severe obstructive sleep apnea. Sleep Breath. 2008; 11. 12(4):393–396. PMID: 18516638.
Article10. Sin DD, Mayers I, Man GC, Pawluk L. Long-term compliance rates to continuous positive airway pressure in obstructive sleep apnea: a population-based study. Chest. 2002; 2. 121(2):430–435. PMID: 11834653.11. Gay P, Weaver T, Loube D, Iber C, et al. Positive Airway Pressure Task Force. Standards of Practice Committee. Evaluation of positive airway pressure treatment for sleep related breathing disorders in adults. Sleep. 2006; 3. 29(3):381–401. PMID: 16553025.
Article12. Kushida CA, Littner MR, Hirshkowitz M, Morgenthaler TI, Alessi CA, Bailey D, et al. Practice parameters for the use of continuous and bilevel positive airway pressure devices to treat adult patients with sleep related breathing disorders. Sleep. 2006; 3. 01. 29(3):375–380. PMID: 16553024.13. Kribbs NB, Pack AI, Kline LR, Smith PL, Schwartz AR, Schubert NM, et al. Objective measurement of patterns of nasal CPAP use by patients with obstructive sleep apnea. Am Rev Respir Dis. 1993; 4. 147(4):887–895. PMID: 8466125.
Article14. Stepnowsky CJ Jr, Moore PJ. Nasal CPAP treatment for obstructive sleep apnea: developing a new perspective on dosing strategies and compliance. J Psychosom Res. 2003; 6. 54(6):599–605. PMID: 12781315.15. Hukins C. Comparative study of autotitrating and fixed-pressure CPAP in the home: a randomized, single-blind crossover trial. Sleep. 2004; 12. 27(8):1512–1517. PMID: 15683142.
Article16. Malhotra A, White DP. Obstructive sleep apnoea. Lancet. 2002; 7. 360(9328):237–245. PMID: 12133673.
Article17. Happel A, Domanski U, Ruhle KH. Pressure-relief continuous positive airway pressure vs constant continuous positive airway pressure: a comparison of efficacy and compliance. Chest. 2006; 10. 130(4):1018–1024. PMID: 17035433.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Treatment of Obstructive Sleep Apnea with Positive Pressure Ventilation
- Surgical Treatment of Adult Obstructive Sleep Apnea
- Improving Compliance for Continuous Positive Airway Pressure Compliance and Possible Influencing Factors
- The Impact of Depressive Symptom on Efficacy and Compliance of Positive Airway Pressure in Obstructive Sleep Apnea
- The Role of Endothelin-1 in Obstructive Sleep Apnea Syndrome and Pulmonary Hypertension