J Korean Soc Radiol.
2010 May;62(5):501-509. 10.3348/jksr.2010.62.5.501.
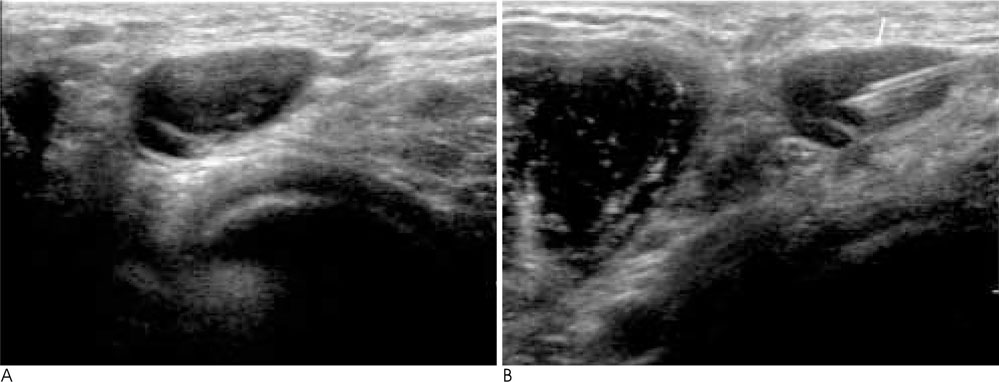
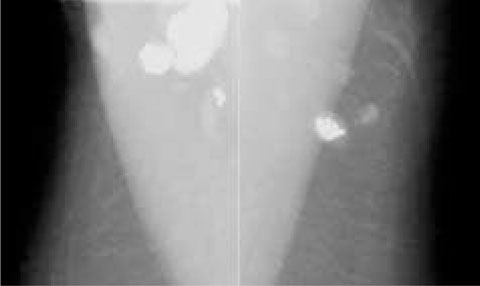
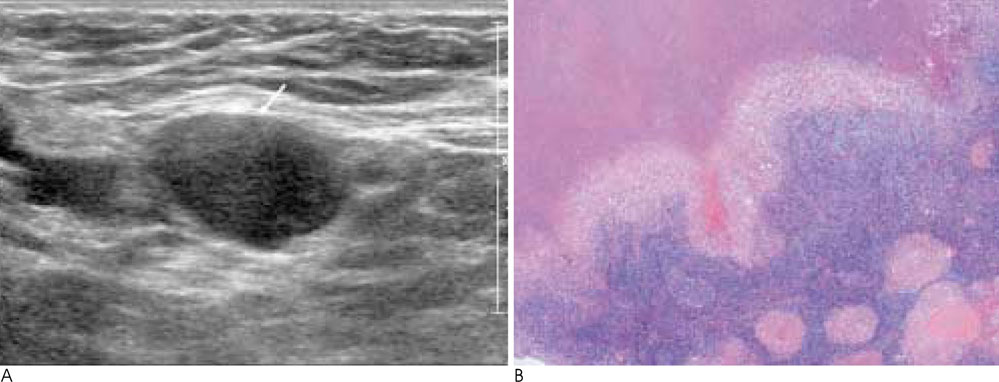
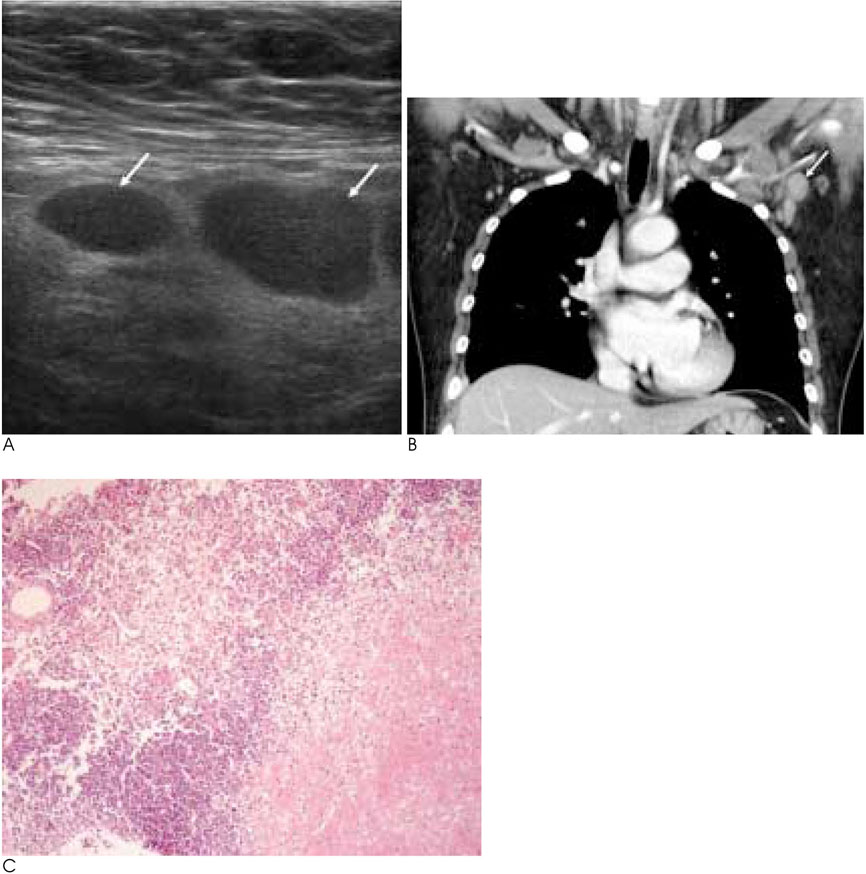
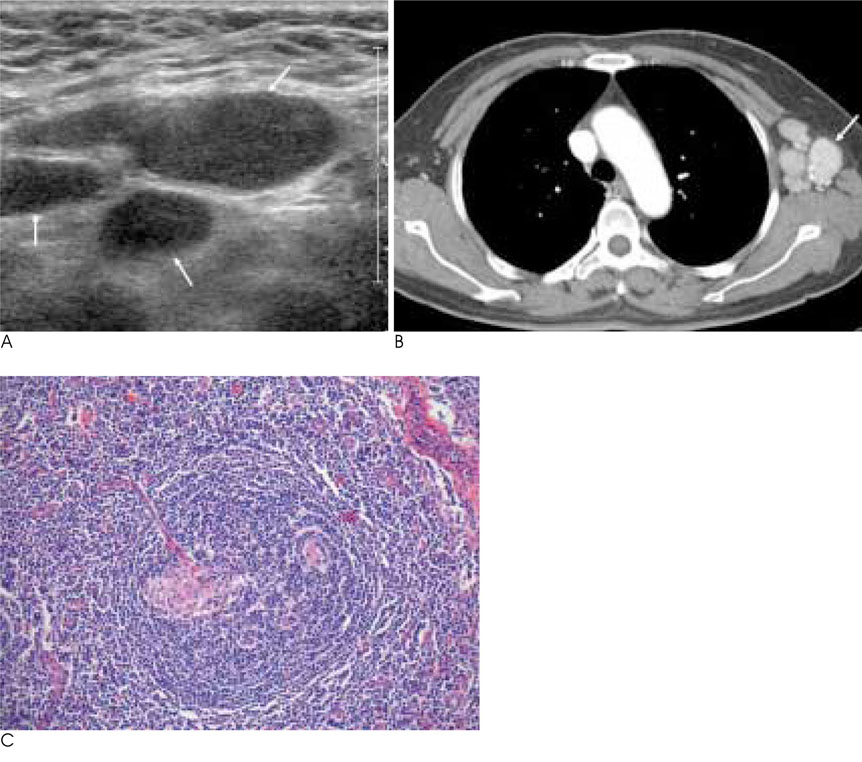
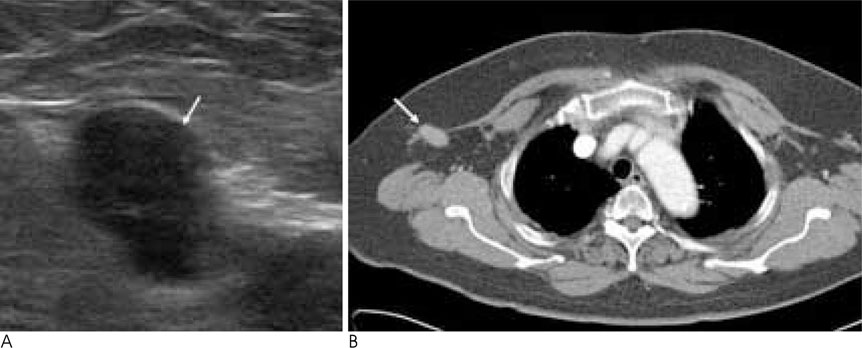
Radiologic Findings of Various Diseases of the Axillary Lymph Node with Pathologic Correlations
- Affiliations
-
- 1Department of Radiology, Soonchunhyang University Hospital, Korea. ywchang@hosp.sch.ac.kr
- 2Department of Radiology, Soonchunhyang Cheonan Hospital, Korea.
- 3Department of Pathology, Soonchunhyang University Hospital, Korea.
- 4Department of Radiology, Soonchunhyang Gumi Hospital, Korea.
- KMID: 2002961
- DOI: http://doi.org/10.3348/jksr.2010.62.5.501
Abstract
- Axillary lymphadenopathy has multiple variable pathologic conditions such as a malignant or benign condition. It is important that we determine the radiologic findings of malignant lymphadenopathy and in turn determine the further course of evaluation for the lesion, because metastatic axillary lymphadenopathy represents an important prognostic factor. Recently, an ultrasonographic-guided axillary lymph node biopsy has been widely used as a diagnostic tool. We discuss the radiologic and pathologic findings of variable axilla diseases and outline the specific findings for determining the results of a lymph node biopsy.
Figure
Reference
-
1. Abe H, Schmidt RA, Sennett CA, Shimauchi A, Newstead GM. US-guided core needle biopsy of axillary lymph nodes in patients with breast cancer: why and How to do it. Radiographics. 2007; 27:S91–S99.2. Lee JY, Kim EK, Kim MJ, Youk JH, Oh KK. Imaging findings of palpable benign masses in axilla. J Korean Soc Ultrasound Med. 2006; 25:21–29.3. Shetty MK, Carpenter WS. Sonographic evaulation of isolated abnormal axillary lymph nodes identified on mammography. J Ultrasound Med. 2004; 23:63–71.4. Yang WT, Chang J, Metreweli C. Patients wit breast cancer: differences in color Doppler flow and gray-scale US features of benign and malignant axillary lymph nodes. Radiology. 2000; 215:568–573.5. Abe H, Schmidt RA, kulkarni K, Sennet CA, Mueller JS, Newstead GM. Axillary lymph nodes suspicious for breast cancer metastasis: sampling with US-guided 14-gauge core-needle biopsy-clinical experience in 100 patients. Radiology. 2009; 250:41–49.6. Deurloo EE, Tanis PJ, Gilhije KG, Muller SH, Kröger R, Peterse JL, et al. Reduction in the number of sentinel lymph node procedures by preoperative ultrasonography of the axilla in breast cancer. Eur J Cancer. 2003; 39:1068–1073.7. Muttarak M, Pojchamarnwiputh S, Chaiwun B. Mammographic features of tuberculous axillary lymphadenitis. Australas Radiol. 2002; 46:260–263.8. Kim HJ, Kim KW, Park YS, Chung DJ, Cho YJ, Hwang CM, et al. Spectrum of axillary disorders (Excluding metastasis from breast cancer): radiolgical and pathological correlation: a pictorial essay. J Korean Radiol Soc. 2007; 57:583–594.9. Youk JH, Kim EK, Ko KH, Kim MJ. Sonographic features of axillary lymphadenopathy caused by kikuchi disease. J Ultrasound Med. 2008; 27:847–853.10. Kwon SY, Kim TK, Kim YS, Lee KY, Lee NJ, Seol HY. CT findings in kikuchi disease: analysis of 96 cases. AJNR Am J Neuroradiol. 2004; 25:1099–1102.11. Bui-Mansfield LT, Chew FS, Myers CP. Angiofollicular lymphoid hyperplasia (Castleman disease) of the axilla. AJR Am J Roentgenol. 2000; 174:1060.12. Eapen M, Mathew CF, Aravindan KP. Evidence based criteria for the histopathological diagnosis of toxoplasmic lymphadenopathy. J Clin Pathol. 2005; 58:1143–1146.13. Ridder GJ, Boedeker CC, Lee TK, Sander A. B-mode sonographic criteria for differential diagnosis of cervicofacial lymphadenopathy in cat-scratch disease and toxoplasmosis. Head Neck. 2003; 25:306–312.14. Shin JH, Choi HY, Moon BI, Sung SH. In vitro sonographic evaluation of sentinel lymph nodes for detecting metastasis in breast cancer: comparison with histopathologic results. J Ultrasound Med. 2004; 23:923–928.15. Bedi DG, Krishnamurthy R, Krishnamurthy S, Edeiken BS, Le Petross H, Fornage BD, et al. Cortical Morphologic features of axillary lymph nodes as a predictor of metastasis in breast cancer: in vitro sonographic study. AJR Am J Roentgenol. 2008; 191:646–652.16. Sapino A, Cassoni P, Zanon E, Fraire F, Croce S, Coluccia C, et al. Ultrasonographically-guided fine-needle aspiration of axillary lymph nodes: role in breast cancer management. Br J Cancer. 2003; 88:702–706.17. Uematsu T, Sano M, Homma K. In vitro high resolution helical CT of small axillary lymph nodes in patients with breast cancer: correlation of CT and histology. AJR Am J Roentgenol. 2001; 176:1069–1074.18. Oran I, Memis A, Ustun EE. Ultrasonographic detection of interpectoral (Rotter's) node involvement in breast cancer. J Clin Ultrasound. 1996; 24:519–522.19. Easson AM, Rotstein LE, Mccready DR. Lymph node assessment in melanoma. J Surg Oncol. 2009; 99:176–185.20. Schaefer NG, Hany TF, Taverna C, Seifert B, Stumpe KD, von Schulthess GK, et al. Non-Hodgkin lymphoma and Hodgkin disease: coregistered FDG PET and CT at staging and restaging-do we need contrast-enhanced CT? Radiology. 2004; 232:823–829.21. Uesato M, Miyazawa Y, Gunji Y, Ochiai T. Primary non-Hodgkin’ s lymphoma of the breast: report of a case with special reference to 380 cases in the japaneses literature. Breast Cancer. 2005; 12:154–158.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Ultrasonography for Staging Axillary Lymph Node in Breast Cancer Patients
- The Efficacy of Sentinel Lymph Node Biopsy Using Radioisotopes in Breast Cancer Patients
- Axillary Lymph-Node Metastases in Patients with T1 Breast Cancer
- Factors related with Axillary Lymph Nodes Metastases in T1 invasive ductal carcinomas of the Breast
- Incidence of Axillary Lymph Node Metastases in T1 Breast Cancer