J Korean Soc Radiol.
2013 Jun;68(6):463-472. 10.3348/jksr.2013.68.6.463.
Characteristics of Consolidation, Centrilobular Nodule and Bronchus as CT Findings for the Differentiation between Tuberculosis and Pneumonia
- Affiliations
-
- 1Department of Radiology, Bucheon St. Mary's Hospital, The Catholic University of Korea College of Medicine, Bucheon, Korea. selene1209@catholic.ac.kr
- 2Department of Radiology, St. Paul's Hospital, The Catholic University of Korea College of Medicine, Seoul, Korea.
- 3Department of Clinical Laboratory Medicine, Bucheon St. Mary's Hospital, The Catholic University of Korea College of Medicine, Bucheon, Korea.
- KMID: 2002897
- DOI: http://doi.org/10.3348/jksr.2013.68.6.463
Abstract
- PURPOSE
To differentiate tuberculosis from pneumonia by computed tomography (CT) in cases difficult to diagnose clinically and radiologically.
MATERIALS AND METHODS
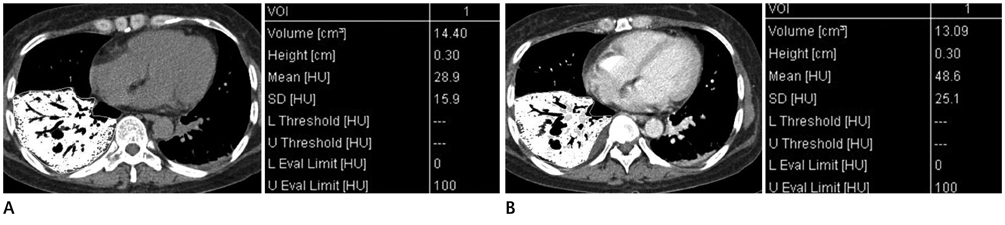
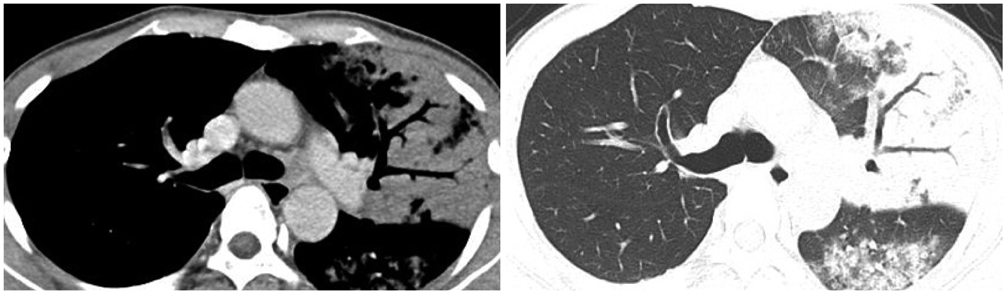
CT scans of 300 patients with tuberculosis and 234 patients with pneumonia were retrospectively analyzed. Parenchymal abnormalities, lymph nodes, pleural effusions and central bronchial narrowing were evaluated. The density of consolidation was measured by pre- and post-enhanced CT.
RESULTS
Centrilobular nodules, granulomas, cavitations in both nodules as well as consolidation, conglomerated nodules, and enlarged lymph nodes occurred with significantly greater frequency in patients with tuberculosis than in those with pneumonia. Centrilobular nodules were larger and denser in tuberculosis patients. In consolidation, decreases in lung lobe volume and a bronchial beaded appearance (irregular narrowing and dilatation) were more frequent in patients with tuberculosis. The tuberculous consolidation had significantly lower mean enhancement and net enhancement than that from pneumonia. When the diagnostic criteria for tuberculosis were set as well-demarcated larger centrilobular nodules and/or a lowerly enhancing consolidation with internal beaded bronchi, the diagnostic accuracy was found to be 82.0%.
CONCLUSION
Consolidation with a low level of enhancement, decreased lung lobe volume, and bronchi with irregular, beaded shape and denser and larger centrilobular nodules are helpful CT findings for the diagnosis of tuberculosis.
MeSH Terms
Figure
Reference
-
1. Burrill J, Williams CJ, Bain G, Conder G, Hine AL, Misra RR. Tuberculosis: a radiologic review. Radiographics. 2007; 27:1255–1273.2. Leung AN. Pulmonary tuberculosis: the essentials. Radiology. 1999; 210:307–322.3. WHO global tuberculosis control report 2010. Summary. Cent Eur J Public Health. 2010; 18:237.4. Ikezoe J, Takeuchi N, Johkoh T, Kohno N, Tomiyama N, Kozuka T, et al. CT appearance of pulmonary tuberculosis in diabetic and immunocompromised patients: comparison with patients who had no underlying disease. AJR Am J Roentgenol. 1992; 159:1175–1179.5. Lee KS, Song KS, Lim TH, Kim PN, Kim IY, Lee BH. Adult-onset pulmonary tuberculosis: findings on chest radiographs and CT scans. AJR Am J Roentgenol. 1993; 160:753–758.6. Arslan O, Gürman G, Dilek I, Ozcan M, Koç H, Ilhan O, et al. Incidence of tuberculosis after bone marrow transplantation in a single center from Turkey. Haematologia (Budap). 1998; 29:59–62.7. Fishman JE, Saraf-Lavi E, Narita M, Hollender ES, Ramsinghani R, Ashkin D. Pulmonary tuberculosis in AIDS patients: transient chest radiographic worsening after initiation of antiretroviral therapy. AJR Am J Roentgenol. 2000; 174:43–49.8. Kim HY, Im JG, Goo JM, Lee JK, Song JW, Kim SK. Pulmonary tuberculosis in patients with systematic lupus erythematosus. AJR Am J Roentgenol. 1999; 173:1639–1642.9. Jeong YJ, Lee KS. Pulmonary tuberculosis: up-to-date imaging and management. AJR Am J Roentgenol. 2008; 191:834–844.10. Miller WT, MacGregor RR. Tuberculosis: frequency of unusual radiographic findings. AJR Am J Roentgenol. 1978; 130:867–875.11. Moon WK, Im JG, Yeon KM, Han MC. Tuberculosis of the central airways: CT findings of active and fibrotic disease. AJR Am J Roentgenol. 1997; 169:649–653.12. Kim Y, Lee KS, Yoon JH, Chung MP, Kim H, Kwon OJ, et al. Tuberculosis of the trachea and main bronchi: CT findings in 17 patients. AJR Am J Roentgenol. 1997; 168:1051–1056.13. Im JG, Itoh H, Shim YS, Lee JH, Ahn J, Han MC, et al. Pulmonary tuberculosis: CT findings--early active disease and sequential change with antituberculous therapy. Radiology. 1993; 186:653–660.14. Rossi SE, Franquet T, Volpacchio M, Giménez A, Aguilar G. Tree-in-bud pattern at thin-section CT of the lungs: radiologic-pathologic overview. Radiographics. 2005; 25:789–801.15. Sochocky S. Tuberculoma of the lung. Am Rev Tuberc. 1958; 78:403–410.16. Jeong YJ, Lee KS, Jeong SY, Chung MJ, Shim SS, Kim H, et al. Solitary pulmonary nodule: characterization with combined wash-in and washout features at dynamic multi-detector row CT. Radiology. 2005; 237:675–683.17. Corley DE, Winterbauer RH. Infectious diseases that result in slowly resolving and chronic pneumonia. Semin Respir Infect. 1993; 8:3–13.18. McCullers JA, Tuomanen EI. Molecular pathogenesis of pneumococcal pneumonia. Front Biosci. 2001; 6:D877–D889.19. Barnes PF, Cave MD. Molecular epidemiology of tuberculosis. N Engl J Med. 2003; 349:1149–1156.20. Rosati LA, Leslie KO. Lung infections. In : Leslie KO, Wick MR, editors. Practical pulmonary pathology; a diagnostic approach. 1st ed. Philadelphia: Churchill Livingstone;2005. p. 97–180.21. Centers for Disease Control (CDC). Update: tuberculosis elimination--United States. MMWR Morb Mortal Wkly Rep. 1990; 39:153–156.22. Bloch AB, Rieder HL, Kelly GD, Cauthen GM, Hayden CH, Snider DE Jr. The epidemiology of tuberculosis in the United States. Implications for diagnosis and treatment. Clin Chest Med. 1989; 10:297–313.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Erratum: Characteristics of Consolidation, Centrilobular Nodule and Bronchus as CT Findings for the Differentiation between Tuberculosis and Pneumonia
- Pulmonary Tuberculosis with Airspace Consolidation vs Mycoplasma Pneumonia in Adults: High-Resolution CT Findings
- Pulmonary Tuberculosis Involving the Right Middle Lobe of the Lung: CT and Clinical Characteristics
- CT Findings Related to Negative Results of Sputum Smear in Patients with Active Pulmonary Tuberculosis having Multiple Cavities
- CT findings of tracheobronchial tuberculosis