J Korean Acad Prosthodont.
2012 Jul;50(3):176-183. 10.4047/jkap.2012.50.3.176.
The success rate of Mg-incorporated oxidized implants in partially edentulous patients: a prospective clinical study
- Affiliations
-
- 1Department of Prosthodontics, School of Dentistry, Kyungpook National University, Daegu, Korea.
- 2Department of Oral and Maxillofacial Surgery, School of Dentistry, Kyungpook National University, Daegu, Korea. vocaloe@knu.ac.kr
- KMID: 2000206
- DOI: http://doi.org/10.4047/jkap.2012.50.3.176
Abstract
- PURPOSE
This study examined the clinical success rate of Mg titanate implants (M Implant system, Shinhung, Korea), which employ a Mg coating method, by evaluating the marginal bone loss and implant stability using radiographs and Osstell(R), over a 1 year.
MATERIALS AND METHODS
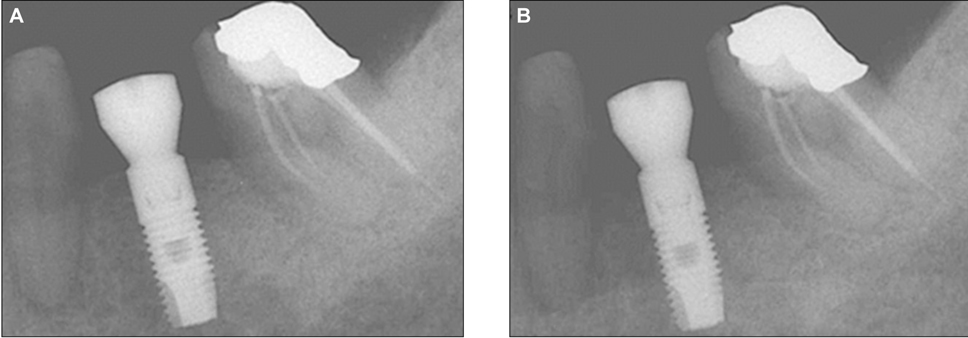
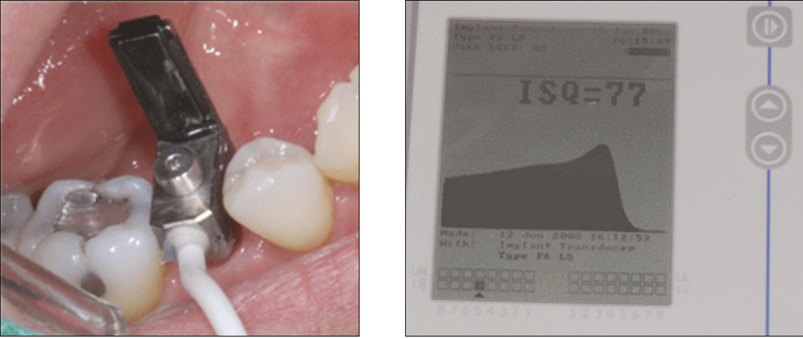
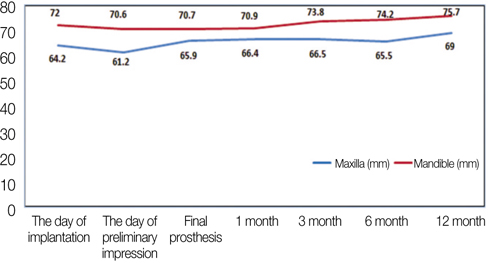
The locations of the implants placement were divided into 4 areas; the maxillary and mandibular premolars and molars. In the maxilla, 8 and 9 implants were inserted in the premolar and molar areas, respectively. In the mandible, 11 and 51 implants were inserted in the premolar and molar areas. Marginal bone loss and ISQ of all implants (79) were measured after insertion, mounting the prosthetic appliance, and 1, 3, 6, and 12 months after loading. The marginal bone loss was measured from the radiograph using XCP bite, which was customized, and the implant stability measured using Osstell(R). Fisher's exact test (alpha=.05) was used to compare the success rates of each region.
RESULTS
The mean marginal bone loss for the upper and lower jaws were 1.537 mm and 1.172 mm. The mobility showed a non-significant reduction or increase according with time. The success rates were accounted for 94.12% and 98.39% in the upper and lower jaws; the premolars and molars were accounted for 100% and 96.67%. The two cases of early failure resulted from failure of primary stability during implant insertion. The late failures were not observed for 1 year after adding a loading to the implants.
CONCLUSION
The Mg titanate implant showed good primary stability and good clinical results in both healing and function.
Keyword
Figure
Reference
-
1. Adell R, Lekholm U, Rockler B, Brånemark PI. A 15-year study of osseointegrated implants in the treatment of the edentulous jaw. Int J Oral Surg. 1981. 10:387–416.
Article2. Albrektsson T, Zarb G, Worthington P, Eriksson AR. The long-term efficacy of currently used dental implants: a review and proposed criteria of success. Int J Oral Maxillofac Implants. 1986. 1:11–25.3. Cox JF, Zarb GA. The longitudinal clinical efficacy of osseointegrated dental implants: a 3-year report. Int J Oral Maxillofac Implants. 1987. 2:91–100.4. Brånemark PI, Hansson BO, Adell R, Breine U, Lindström J, Hallén O, Ohman A. Osseointegrated implants in the treatment of the edentulous jaw. Experience from a 10-year period. Scand J Plast Reconstr Surg Suppl. 1977. 16:1–132.5. Brånemark PI. Brånemark PI, Zarb GA, Albrektsson T, editors. Introduction to osseointegration. Tissue-Integrated Prosthese. Osseointegration in Clinical Dentistry. 1985. Chicago; IL: Quintessence Publishing Co, Inc..6. Albrektsson TO, Johansson CB, Sennerby L. Biological aspects of implant dentistry: osseointegration. Periodontol 2000. 1994. 4:58–73.
Article7. Zarb GA, Albrektsson T. Osseointegration: A requiem for the periodontal ligament? Int J Periodont Res Dent. 1991. 11:88–91.8. Albrektsson T, Dahl E, Enbom L, Engevall S, Engquist B, Eriksson AR, Feldmann G, Freiberg N, Glantz PO, Kjellman O, et al. Osseointegrated oral implants. A Swedish multicenter study of 8139 consecutively inserted Nobelpharma implants. J Periodontol. 1988. 59:287–296.9. Adell R, Eriksson B, Lekholm U, Brånemark PI, Jemt T. Long-term follow-up study of osseointegrated implants in the treatment of totally edentulous jaws. Int J Oral Maxillofac Implants. 1990. 5:347–359.10. Johansson C, Albrektsson T. Integration of screw implants in the rabbit: a 1-year follow-up of removal torque of titanium implants. Int J Oral Maxillofac Implants. 1987. 2:69–75.11. Tjellström A, Jacobsson M, Albrektsson T. Removal torque of osseointegrated craniofacial implants: a clinical study. Int J Oral Maxillofac Implants. 1988. 3:287–289.12. Adell R, Lekholm U, Rockler B, Brånemark PI, Lindhe J, Eriksson B, Sbordone L. Marginal tissue reactions at osseointegrated titanium fixtures (I). A 3-year longitudinal prospective study. Int J Oral Maxillofac Surg. 1986. 15:39–52.13. Zarb GA, Schmitt A. The longitudinal clinical effectiveness of osseointegrated dental implants: the Toronto study. Part III: Problems and complications encountered. J Prosthet Dent. 1990. 64:185–194.
Article14. Sundén S, Gröndahl K, Gröndahl HG. Accuracy and precision in the radiographic diagnosis of clinical instability in Brånemark dental implants. Clin Oral Implants Res. 1995. 6:220–226.
Article15. Barewal RM, Oates TW, Meredith N, Cochran DL. Resonance frequency measurement of implant stability in vivo on implants with a sandblasted and acid-etched surface. Int J Oral Maxillofac Implants. 2003. 18:641–651.16. Albrektsson T, Brånemark PI, Hansson HA, Lindström J. Osseointegrated titanium implants. Requirements for ensuring a long-lasting, direct bone-to-implant anchorage in man. Acta Orthop Scand. 1981. 52:155–170.
Article17. Carlsson L, Röstlund T, Albrektsson B, Albrektsson T. Removal torques for polished and rough titanium implants. Int J Oral Maxillofac Implants. 1988. 3:21–24.18. Gotfredsen K, Nimb L, Hjörting-Hansen E, Jensen JS, Holmén A. Histomorphometric and removal torque analysis for TiO2-blasted titanium implants. An experimental study on dogs. Clin Oral Implants Res. 1992. 3:77–84.
Article19. Cordioli G, Majzoub Z, Piattelli A, Scarano A. Removal torque and histomorphometric investigation of 4 different titanium surfaces: an experimental study in the rabbit tibia. Int J Oral Maxillofac Implants. 2000. 15:668–674.20. Klokkevold PR, Nishimura RD, Adachi M, Caputo A. Osseointegration enhanced by chemical etching of the titanium surface. A torque removal study in the rabbit. Clin Oral Implants Res. 1997. 8:442–447.
Article21. Wennerberg A, Albrektsson T, Andersson B, Krol JJ. A histomorphometric and removal torque study of screw-shaped titanium implants with three different surface topographies. Clin Oral Implants Res. 1995. 6:24–30.
Article22. Ferguson SJ, Langhoff JD, Voelter K, von Rechenberg B, Scharnweber D, Bierbaum S, Schnabelrauch M, Kautz AR, Frauchiger VM, Mueller TL, van Lenthe GH, Schlottig F. Biomechanical comparison of different surface modifications for dental implants. Int J Oral Maxillofac Implants. 2008. 23:1037–1046.23. Meredith N, Alleyne D, Cawley P. Quantitative determination of the stability of the implant-tissue interface using resonance frequency analysis. Clin Oral Implants Res. 1996. 7:261–267.
Article24. Tonetti MS, Schmid J. Pathogenesis of implant failures. Periodontol 2000. 1994. 4:127–138.
Article25. Sul YT, Byon E, Wennerberg A. Surface characteristics of electrochemically oxidized implants and acid-etched implants: surface chemistry, morphology, pore configurations, oxide thickness, crystal structure, and roughness. Int J Oral Maxillofac Implants. 2008. 23:631–640.26. Sul YT, Jeong Y, Johansson C, Albrektsson T. Oxidized, bioactive implants are rapidly and strongly integrated in bone. Part 1-experimental implants. Clin Oral Implants Res. 2006. 17:521–526.
Article27. Sul YT, Johansson C, Byon E, Albrektsson T. The bone response of oxidized bioactive and non-bioactive titanium implants. Biomaterials. 2005. 26:6720–6730.
Article28. Sul YT, Johansson C, Wennerberg A, Cho LR, Chang BS, Albrektsson T. Optimum surface properties of oxidized implants for reinforcement of osseointegration: surface chemistry, oxide thickness, porosity, roughness, and crystal structure. Int J Oral Maxillofac Implants. 2005. 20:349–359.29. Sennerby L, Meredith N. Resonance frequency analysis: measuring implant stability and osseointegration. Compend Contin Educ Dent. 1998. 19:493–498. 50050230. Meredith N, Book K, Friberg B, Jemt T, Sennerby L. Resonance frequency measurements of implant stability in vivo. A cross-sectional and longitudinal study of resonance frequency measurements on implants in the edentulous and partially dentate maxilla. Clin Oral Implants Res. 1997. 8:226–233.
Article31. Rasmusson L, Meredith N, Cho IH, Sennerby L. The influence of simultaneous versus delayed placement on the stability of titanium implants in onlay bone grafts. A histologic and biomechanic study in the rabbit. Int J Oral Maxillofac Surg. 1999. 28:224–231.
Article32. Huang HM, Chiu CL, Yeh CY, Lee SY. Factors influencing the resonance frequency of dental implants. J Oral Maxillofac Surg. 2003. 61:1184–1188.
Article33. Sul YT, Johansson C, Albrektsson T. Which surface properties enhance bone response to implants? Comparison of oxidized magnesium, TiUnite, and Osseotite implant surfaces. Int J Prosthodont. 2006. 19:319–328.34. Sul YT, Johansson P, Chang BS, Byon ES, Jeong Y. Bone tissue responses to Mg-incorporated oxidized implants and machine-turned implantsin the rabbit femur. J Appl Biomater Biomech. 2005. 3:18–28.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- LONGITUDINAL CLINICAL STUDY ON THE EFFICACY OF OSSEOINTEGRATED DENTAL IMPLANTS IN PARTIALLY EDENTULOUS KOREAN PATIENTS
- COMPARISON OF RESONANCE FREQUENCY ANALYSIS BETWEEN VARIOUS SURFACE PROPERTIES
- Randomized controlled clinical trial of 2 types of hydroxyapatite-coated implants on moderate periodontitis patients
- Results of immediate loading for implant restoration in partially edentulous patients: a 6-month preliminary prospective study using SinusQuick(TM) EB implant system
- A 5-year prospective clinical study of Neobiotech implants for partially edentulous patients