Korean J Urol.
2007 Nov;48(11):1174-1178. 10.4111/kju.2007.48.11.1174.
Primary Leiomyosarcoma of the Ureter
- Affiliations
-
- 1Department of Urology, Konyang University College of Medicine, Daejeon, Korea. urohan@kyuh.co.kr
- KMID: 1997097
- DOI: http://doi.org/10.4111/kju.2007.48.11.1174
Abstract
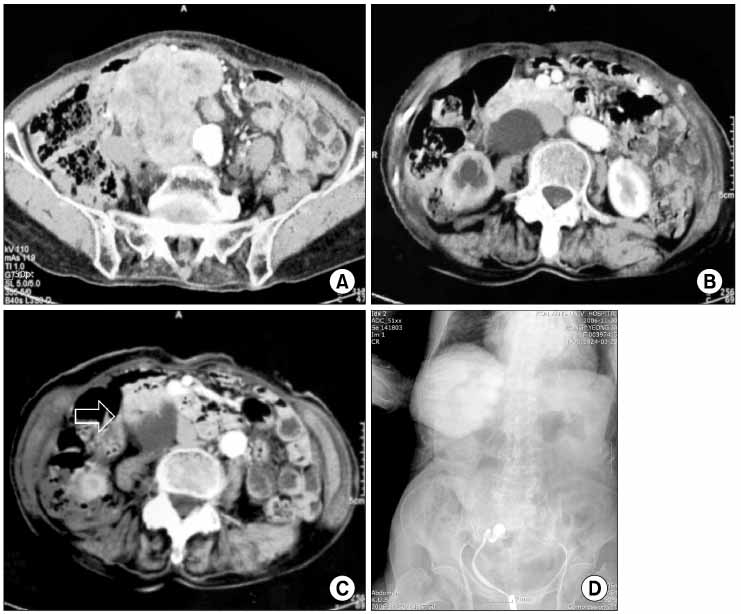
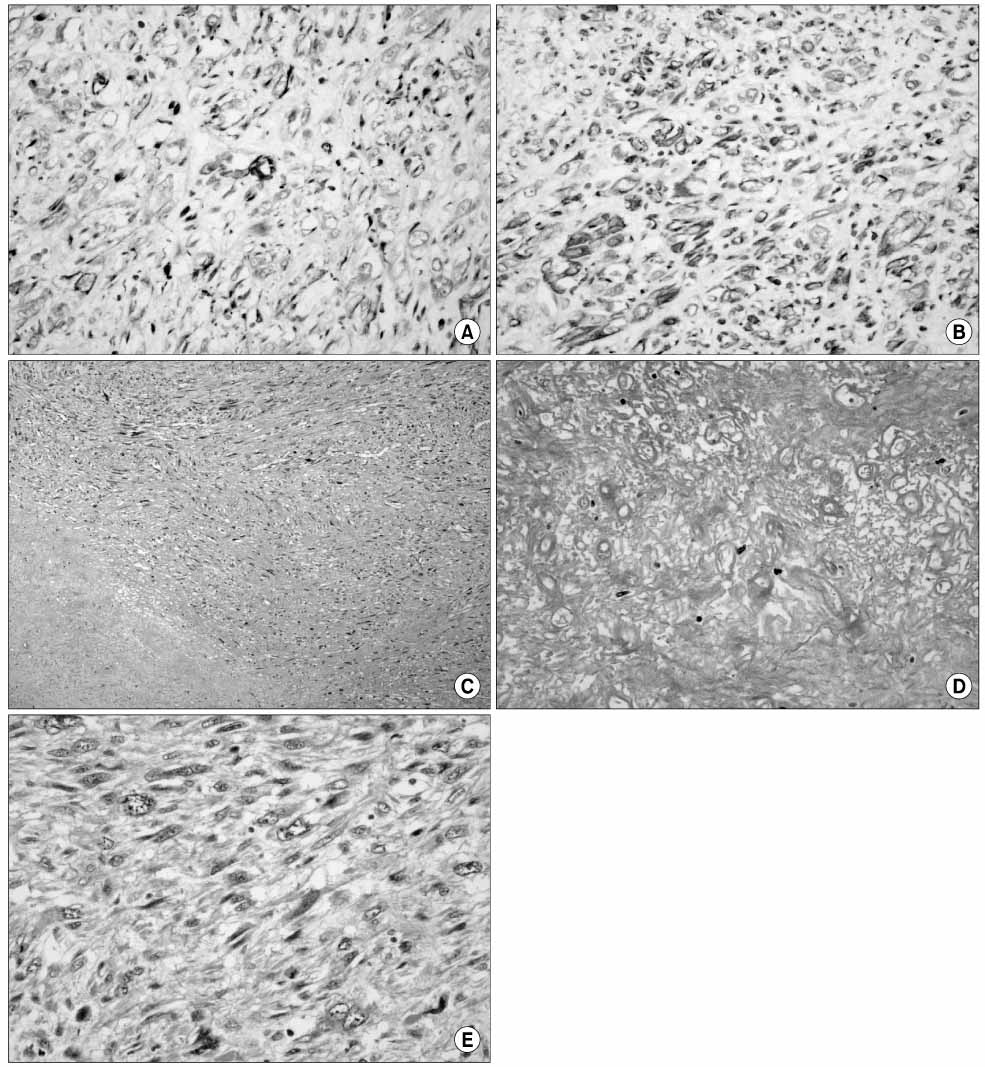
- An 82-year-old woman was admitted to our hospital with a palpable mass in her right lower abdomen. The mass was enlarged and tender for the previous 3 months. Abdomen-pelvic computed tomographic scan demonstrated severe right hydroureteronephrosis and about an 8x8x9cm sized huge irregular shaped pelvic mass. Retrograde pyelography showed complete obstruction of the right middle ureter. En bloc resection of the mass and segmental resection of the ureter was performed. Pathologically, it was diagnosed primary leiomyosarcoma of the ureter. At 3 month postoperatively, there has been no recurrence or metastasis.
Keyword
MeSH Terms
Figure
Reference
-
1. Abeshouse BS. Primary benign and malignant tumors of the ureter: a review of the literature and report of one benign and twelve malignant tumors. Am J Surg. 1956. 91:237–271.2. Hashimoto H, Tsuneyoshi M, Enjoji M. Malignant smooth muscle tumors of the retroperitoneum and mesentery: a clinicopathologic analysis of 44 cases. J Surg Oncol. 1985. 28:177–186.3. Shirotake S, Sumitomo M, Asakuma J, Asano T, Aiko S, Hayakawa M. A case of primary leiomyosarcoma of the ureter. Hinyokika Kiyo. 2006. 52:41–45.4. Griffin JH, Waters WB. Primary leiomyosarcoma of the ureter. J Surg Oncol. 1996. 62:148–152.5. Raut CP, Pisters PW. Retroperitoneal sarcomas: combinedmodality treatment approaches. J Surg Oncol. 2006. 94:81–87.6. Nakajima F, Terahata S, Hatano T, Nishida K. Primary leiomyosarcoma of the ureter. Urol Int. 1994. 53:166–168.7. Moon DS, Kim HS, Park YI, Min BK. A case of retroperitoneal leiomyosarcoma. Korean J Urol. 1989. 30:430–433.8. An HJ, Woo JW, Lee CK, Rhew HY. A case of retroperitoneal leiomyosarcoma. Korean J Urol. 1999. 40:526–528.9. Gislason T, Arnarson OO. Primary ureteral leiomyosarcoma. Scand J Urol Nephrol. 1984. 18:253–254.10. Rosenberg A. Cotran RS, Kumar V, Collins T, editors. Bones, joints, and soft tissue tumors. Pathologic basis of disease. 1999. 6th ed. Philadelphia: Saunders;1215–1268.