Korean J Urol.
2010 Aug;51(8):537-543. 10.4111/kju.2010.51.8.537.
Accuracy of Methods for Urinary Detection in Women with Stress Urinary Incontinence
- Affiliations
-
- 1Department of Urology, Inha University College of Medicine, Incheon, Korea. lt11@inha.ac.kr
- 2Department of Social and Preventive Medicine, Inha University College of Medicine, Incheon, Korea.
- 3Department of Urology, Inha University Graduate School of Medicine, Incheon, Korea.
- KMID: 1997021
- DOI: http://doi.org/10.4111/kju.2010.51.8.537
Abstract
- PURPOSE
We assessed the accuracy of urinary detection by visualization compared with a method using the urethral channel of a transurethral, three-channel urodynamic catheter.
MATERIALS AND METHODS
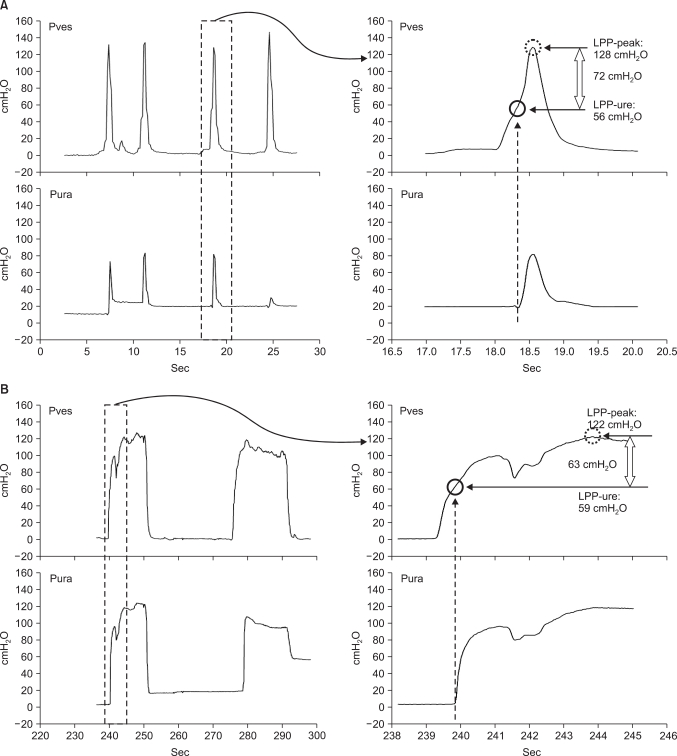
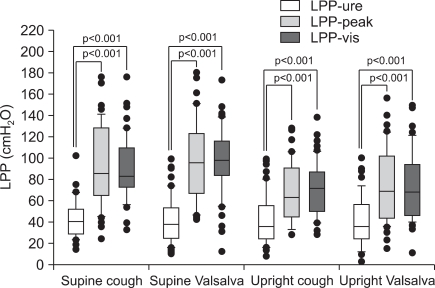
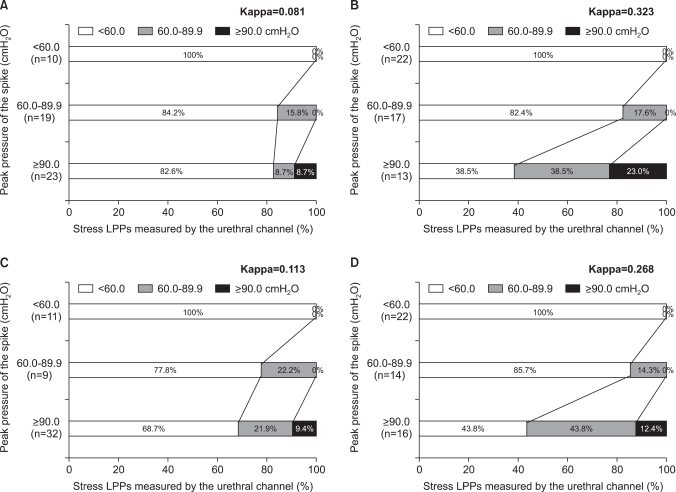
This was a case series of 52 patients presenting with stress urinary incontinence over 2 years. Patients underwent video-urodynamic studies in both the supine and the erect positions by use of two techniques for measuring leak point pressure (LPP) by one examiner. LPP was determined as the intravesical pressure simultaneous to the starting point of urethral pressure changes through the urethral channel of a urodynamic catheter (LPP-ure) and then by visualization (LPP-vis) during different events. We also measured the time related to the provocations and the time to mark the leakage on the urodynamic machine by the examiner.
RESULTS
The LPP-ure values (cough supine: 42.1+/-18.7, cough erect: 42.1+/-21.8, Valsalva supine: 42.2+/-23.3, Valsalva erect: 41.0+/-22.6 cmH2O) were significantly lower than the LPP-vis values (89.9+/-29.4, 97.4+/-30.4, 70.6+/-25.2, and 74.4+/-32.6 cmH2O, respectively, all p<0.001). Whereas the actual leakages happened during the pressure increases, urodynamic recording by visualization was done after those increases had finished.
CONCLUSIONS
The use of visualization as a urinary detection method entails potential errors that cannot be adjusted for on that time scale. Our results emphasize the need to standardize the methodologies used for urinary leakage detection, because this measurement is closely related to the accuracy of measurement of leak point pressure.
Keyword
Figure
Reference
-
1. Bump RC, Elser DM, Theofrastous JP, McClish DK. Valsalva leak point pressures in women with genuine stress incontinence: reproducibility, effect of catheter caliber, and correlations with other measures of urethral resistance. Continence Program for Women Research Group. Am J Obstet Gynecol. 1995; 173:551–557. PMID: 7645634.2. Miklos JR, Sze EH, Karram MM. A critical appraisal of the methods of measuring leak-point pressures in women with stress incontinence. Obstet Gynecol. 1995; 86:349–352. PMID: 7651641.
Article3. Betson LH, Siddiqui G, Bhatia NN. Intrinsic urethral sphincteric deficiency: critical analysis of various diagnostic modalities. Curr Opin Obstet Gynecol. 2003; 15:411–417. PMID: 14501245.
Article4. Lemack GE. Urodynamic assessment of patients with stress incontinence: how effective are urethral pressure profilometry and abdominal leak point pressures at case selection and predicting outcome? Curr Opin Urol. 2004; 14:307–311. PMID: 15626870.
Article5. Theofrastous JP, Cundiff GW, Harris RL, Bump RC. The effect of vesical volume on Valsalva leak-point pressures in women with genuine stress urinary incontinence. Obstet Gynecol. 1996; 87:711–714. PMID: 8677072.
Article6. Nguyen JK, Gunn GC, Bhatia NN. The effect of patient position on leak-point pressure measurements in women with genuine stress incontinence. Int Urogynecol J Pelvic Floor Dysfunct. 2002; 13:9–14. PMID: 11999213.
Article7. Swift SE, Utrie JW. The need for standardization of the valsalva leak-point pressure. Int Urogynecol J Pelvic Floor Dysfunct. 1996; 7:227–230. PMID: 10895809.
Article8. McGuire EJ, Cespedes RD, O'Connell HE. Leak-point pressures. Urol Clin North Am. 1996; 23:253–262. PMID: 8659025.
Article9. McGuire EJ, Fitzpatrick CC, Wan J, Bloom D, Sanvordenker J, Ritchey M, et al. Clinical assessment of urethral sphincter function. J Urol. 1993; 150:1452–1454. PMID: 8411422.
Article10. Culligan PJ, Goldberg RP, Blackhurst DW, Sasso K, Koduri S, Sand PK. Comparison of microtransducer and fiberoptic catheters for urodynamic studies. Obstet Gynecol. 2001; 98:253–257. PMID: 11506841.
Article11. Nygaard I. Physiologic outcome measures for urinary incontinence. Gastroenterology. 2004; 126(1 Suppl 1):S99–S105. PMID: 14978645.
Article12. Versi E, Lyell DJ, Griffiths DJ. Videourodynamic diagnosis of occult genuine stress incontinence in patients with anterior vaginal wall relaxation. J Soc Gynecol Investig. 1998; 5:327–330.
Article13. Kuo HC. Videourodynamic results after pubovaginal sling procedure for stress urinary incontinence. Urology. 1999; 54:802–806. PMID: 10565737.
Article14. Siltberg H, Larsson G, Hallen B, Johansson C, Ulmsten U. Validation of cough-induced leak point pressure measurement in the evaluation of pharmacological treatment of stress incontinence. Neurourol Urodyn. 1999; 18:591–602. PMID: 10529707.
Article15. Abrams P, Blaivas JG, Stanton SL, Andersen JT. The standardisation of terminology of lower urinary tract function. The International Continence Society Committee on Standardisation of Terminology. Scand J Urol Nephrol Suppl. 1988; 114:5–19. PMID: 3201169.16. Bump RC, Mattiasson A, Bo K, Brubaker LP, DeLancey JO, Klarskov P, et al. The standardization of terminology of female pelvic organ prolapse and pelvic floor dysfunction. Am J Obstet Gynecol. 1996; 175:10–17. PMID: 8694033.
Article17. Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977; 33:159–174. PMID: 843571.
Article18. Abrams P, Cardozo L, Fall M, Griffiths D, Rosier P, Ulmsten U, et al. The standardisation of terminology of lower urinary tract function: report from the Standardisation Sub-committee of the International Continence Society. Neurourol Urodyn. 2002; 21:167–178. PMID: 11857671.
Article19. O'Connor RC, Nanigian DK, Lyon MB, Ellison LM, Bales GT, Stone AR. Early outcomes of mid-urethral slings for female stress urinary incontinence stratified by valsalva leak point pressure. Neurourol Urodyn. 2006; 25:685–688. PMID: 16817185.20. Wan J, McGuire EJ, Bloom DA, Ritchey ML. Stress leak point pressure: a diagnostic tool for incontinent children. J Urol. 1993; 150:700–702. PMID: 8326627.
Article21. Kocjancic E, Tarrano E, Panella M, Crivellaro S, Smith JJ 3rd, Maso G, et al. Evaluation of minimally invasive analysis system for cough leak point pressure measurement. J Urol. 2004; 172:994–997. PMID: 15311021.
Article22. Swift SE, Ostergard DR. A comparison of stress leak-point pressure and maximal urethral closure pressure in patients with genuine stress incontinence. Obstet Gynecol. 1995; 85:704–708. PMID: 7724100.
Article23. Siltberg H, Larsson G, Victor A. Cough-induced leak-point pressure--a valid measure for assessing treatment in women with stress incontinence. Acta Obstet Gynecol Scand. 1998; 77:1000–1007. PMID: 9849845.24. Faerber GJ, Vashi AR. Variations in Valsalva leak point pressure with increasing vesical volume. J Urol. 1998; 159:1909–1911. PMID: 9598485.
Article25. Bump RC, Hurt WG, Fantl JA, Wyman JF. Assessment of Kegel pelvic muscle exercise performance after brief verbal instruction. Am J Obstet Gynecol. 1991; 165:322–327. PMID: 1872333.
Article26. Almeida FG, Bruschini H, Srougi M. Correlation between urethral sphincter activity and Valsalva leak point pressure at different bladder distentions: revisiting the urethral pressure profile. J Urol. 2005; 174:1312–1315. PMID: 16145410.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Two Cases of New Operative Technique in Treatment of Stress Urinary Incontinence
- Marshall-Marchetti Operation and Modified Pereyra Procedure for Stress Urinary Incontinence
- The Effect of Pelvic Muscle Exercise Program on Women with Stress Urinary Incontinence in the Degree and Amount of Urinary Incontinence and Maximum Vaginal Contraction Pressure
- Experience of Transvaginal Bladder Neck Suspension(Raz Procedure) for Stress Urinary Incontinence: 10 Cases
- Factors Affecting the Severity of Urinary Incontinence and the Quality of Life of Women with Urinary Incontinence