Korean J Urol.
2012 Jan;53(1):14-17. 10.4111/kju.2012.53.1.14.
Pattern of Lymph Node Metastasis Correlates with Tumor Location in Bladder Cancer
- Affiliations
-
- 1Department of Urology, National Health Insurance Corporation Ilsan Hospital, Goyang, Korea. urokim@nhimc.or.kr
- KMID: 1988817
- DOI: http://doi.org/10.4111/kju.2012.53.1.14
Abstract
- PURPOSE
Resection of a large number of lymph nodes (LNs) increases survival in patients with LN-positive disease; however, morbidity also increases. Here, we investigated the correlation between tumor location and LN metastasis in bladder cancer.
MATERIALS AND METHODS
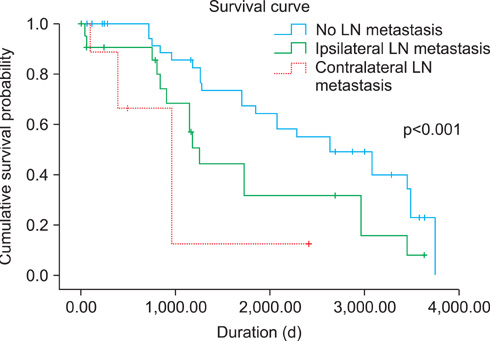
Thirty-six patients with pathological N1 or higher bladder cancer, who underwent radical cystectomy with extended lymphadenectomy, were reviewed retrospectively. The tumor location was classified as right, left, front, posterior, or whole bladder. The LN metastasis pattern was classified as right, left, or bilateral. The correlation between tumor location and LN metastasis was determined by chi-square test. Survival rates were compared by Kaplan-Meier analysis.
RESULTS
The numbers of patients with a tumor on the right (group 1), left (group 2), posterior (group 3), or whole (group 4) bladder were 16 (44.4%), 16 (44.4%), 2 (5.6%), and 2 (5.6%), respectively. In group 1, 14 patients (87.5%) had right-sided ipsilateral LNs, and 2 patients (12.5%) had left-sided contralateral LNs. In group 2, 4 patients (25%) had right-sided contralateral LNs, and 12 patients (75%) had left-sided ipsilateral LNs. In group 3, both patients (100%) had right-sided posterior LNs. In group 4, both patients (100%) had positive LNs on both sides. Tumor location and LN metastasis were significantly correlated (p<0.05). Moreover, the survival rate was significantly higher in patients with no LN metastasis than in patients with ipsilateral or contralateral LN-positive bladder cancer.
CONCLUSIONS
The location of the bladder tumor and direction of metastatic spread were significantly correlated. Mandatory bilateral lymphadenectomy during radical cystectomy should be questioned.
MeSH Terms
Figure
Reference
-
1. Karl A, Carroll PR, Gschwend JE, Knüchel R, Montorsi F, Stief CG, et al. The impact of lymphadenectomy and lymph node metastasis on the outcomes of radical cystectomy for bladder cancer. Eur Urol. 2009. 55:826–835.2. Ku JH. Role of pelvic lymphadenectomy in the treatment of bladder cancer: a mini review. Korean J Urol. 2010. 51:371–378.3. Liedberg F, Månsson W. Lymph node metastasis in bladder cancer. Eur Urol. 2006. 49:13–21.4. Shinagare AB, Ramaiya NH, Jagannathan JP, Fennessy FM, Taplin ME, Van den Abbeele AD. Metastatic pattern of bladder cancer: correlation with the characteristics of the primary tumor. AJR Am J Roentgenol. 2011. 196:117–122.5. Wishnow KI, Johnson DE, Ro JY, Swanson DA, Babaian RJ, von Eschenbach AC. Incidence, extent and location of unsuspected pelvic lymph node metastasis in patients undergoing radical cystectomy for bladder cancer. J Urol. 1987. 137:408–410.6. Herr HW, Donat SM. Outcome of patients with grossly node positive bladder cancer after pelvic lymph node dissection and radical cystectomy. J Urol. 2001. 165:62–64.7. Leissner J, Hohenfellner R, Thüroff JW, Wolf HK. Lymphadenectomy in patients with transitional cell carcinoma of the urinary bladder; significance for staging and prognosis. BJU Int. 2000. 85:817–823.8. Seiler R, von Gunten M, Thalmann GN, Fleischmann A. Pelvic lymph nodes: distribution and nodal tumour burden of urothelial bladder cancer. J Clin Pathol. 2010. 63:504–507.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Pattern of Recurrences and Metastases according to Regional Lymph Node Metastasis of Colorectal Cancer
- Clinical Significance of the Pattern of Lymph Node Metastasis Depending on the Location of Gastric Cancer
- Rare Manifestation of the Cutaneous and Cervical Lymph Node Metastases of Urothelial Carcinoma of Urinary Bladder: A Case Report
- Analysis of Factors Related to Lymph Node Metastasis in Early Gastric Cancers
- The Pattern of Cervical Lymph Node Metastases in Papillary Thyroid Cancer