J Cerebrovasc Endovasc Neurosurg.
2013 Jun;15(2):67-75. 10.7461/jcen.2013.15.2.67.
Impact of Admission Month on Outcomes in Spontaneous Subarachnoid Hemorrhage: Evidence Against the March Effect
- Affiliations
-
- 1Department of Neurosurgery, Gil Medical Center, Incheon, Gachon University, Republic of Korea. cwpark@gilhospital.com
- KMID: 1980432
- DOI: http://doi.org/10.7461/jcen.2013.15.2.67
Abstract
OBJECTIVE
We attempted to identify the presence of a so called 'March effect (or phenomenon)' (which had long been known as a 'July effect' in western countries), a transient increase in adverse outcomes during an unskilled period for new interns and residents in a teaching hospital, among a cohort of patients with spontaneous subarachnoid hemorrhage (sSAH).
METHODS
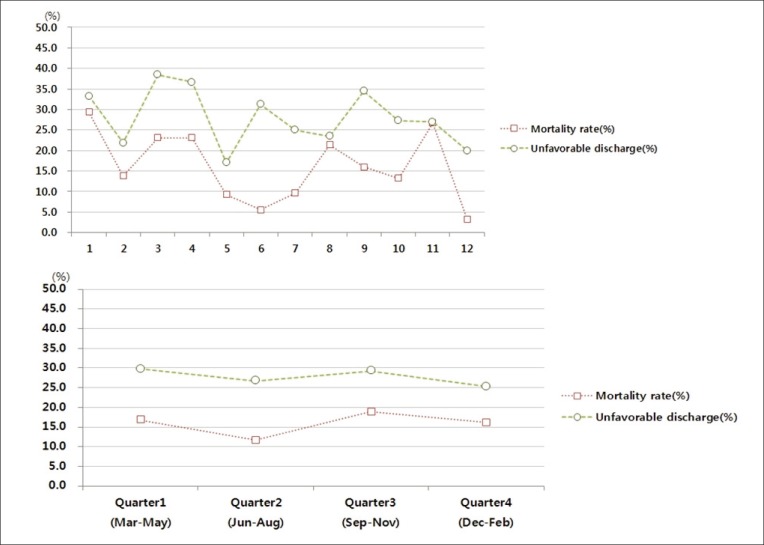
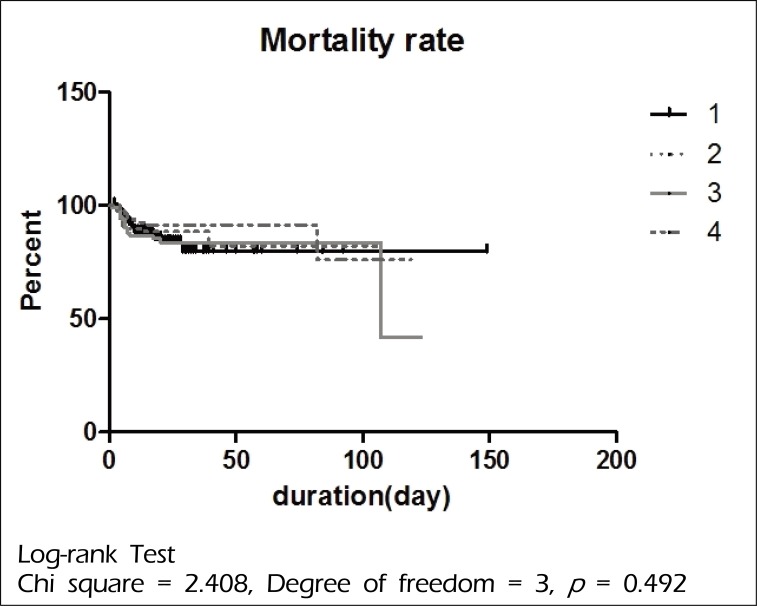
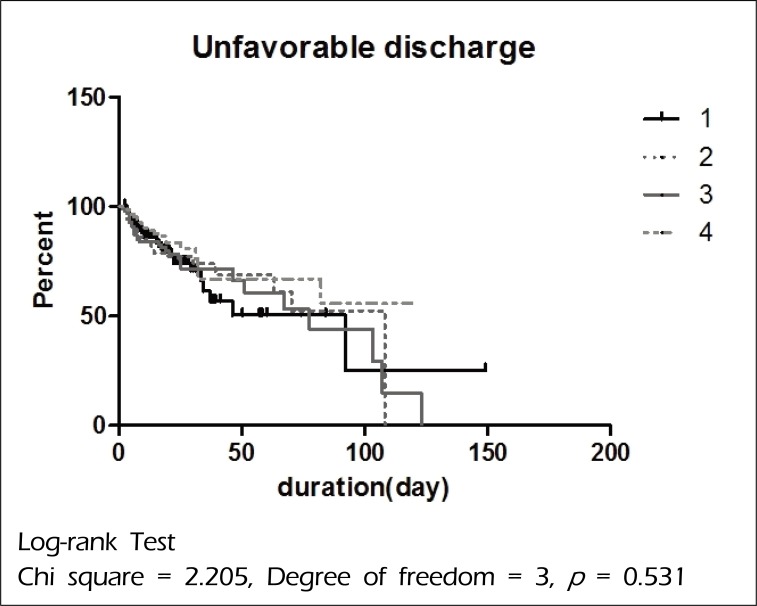
A total of 455 consecutive patients with sSAH from our department database from 2008 to 2010 were enrolled retrospectively and the admission month, patient demographics and clinical characteristics, treatment modalities and discharge outcomes were analyzed. Multivariate regression analysis was used to determine whether unfavorable discharge and in-hospital mortality showed a significant increase during the unskilled months for new interns and residents (from March to May) in a pattern suggestive of a "March effect".
RESULTS
Among 455 patients with sSAH, 113 patients were treated during the unskilled period (from March to May) and the remaining 342 patients were treated during the skilled period (from June until February of the next year). No statistically significant difference in demographics and clinical characteristics was observed between patients treated during these periods. In addition, the mortality and unfavorable discharge rates of the un-skilled period were 16.8% and 29.7% and those of the skilled period were 15.5% and 27.2%, respectively. However, no statistically significant difference was observed between them.
CONCLUSIONS
Findings of our study suggest that there was no 'March effect' on the mortality rate and unfavorable discharge rate among patients with sSAH in our hospital during the study period.
Keyword
MeSH Terms
Figure
Reference
-
1. Aylin P, Majeed FA. The killing season-fact or fiction. BMJ. 1994; 12. 309(6970):1690. PMID: 7819988.
Article2. Banco SP, Vaccaro AR, Blam O, Eck JC, Cotler JM, Hilibrand AS, et al. Spine infections: variations in incidence during the academic year. Spine (Phila Pa 1976). 2002; 5. 27(9):962–965. PMID: 11979171.3. Barger LK, Cade BE, Ayas NT, Cronin JW, Rosner B, Speizer FE, et al. Extended work shifts and the risk of motor vehicle crashes among interns. N Engl J Med. 2005; 1. 352(2):125–134. PMID: 15647575.
Article4. Barry WA, Rosenthal GE. Is there a July phenomenon? The effect of July admissions on intensive care morality and length of stay in teaching hospitals. J Gen Intern Med. 2003; 8. 18(8):639–645. PMID: 12911646.5. Bederson JB, Connolly ES Jr, Batjer HH, Dacey RG, Dion JE, Diringer MN, et al. Guidelines for the management of aneurysmal subarachnoid hemorrhage: a statement for healthcare professionals from a special writing group of the Stroke Council, American Heart Association. Stroke. 2009; 3. 40(3):994–1025. PMID: 19164800.
Article6. Blumberg MS. Measuring surgical quality in Maryland: a model. Health Aff (Millwood). 1988; 2. 7(1):62–78. PMID: 3360395.
Article7. Buchwald D, Komaroff AL, Cook EF, Epstein AM. Indirect costs for medical education. Is there a July phenomenon? Arch Intern Med. 1989; 4. 149(4):765–768. PMID: 2495778.
Article8. Claridge JA, Schulman AM, Sawyer RG, Ghezel-Ayagh A, Young JS. The 'July phenomenon' and the care of the severely injured patient: fact or fiction? Surgery. 2001; 8. 130(2):346–353. PMID: 11490370.
Article9. Davydov L, Caliendo G, Mehl B, Smith LG. Investigation of correlation between house-staff work hours and prescribing errors. Am J Health Syst Pharm. 2004; 6. 61(11):1130–1134. PMID: 15237565.
Article10. Diringer MN. Management of aneurysmal subarachnoid hemorrhage. Crit Care Med. 2009; 2. 37(2):432–440. PMID: 19114880.
Article11. Englesbe MJ, Pelletier SJ, Magee JC, Gauger P, Schifftner T, Henderson WG, et al. Seasonal variation in surgical outcomes as measured by the American College of Surgeons-National Surgical Quality Improvement Program (ACS-NSQIP). Ann Surg. 2007; 9. 246(3):456–462. discussion 463-5. PMID: 17717449.
Article12. Finkielman JD, Moreles J, Peters SG, Keegan MT, Ensminger SA, Lymp JF, et al. Mortality rate and length of stay of patients admitted to the intensive care unit in July. Crit Care Med. 2004; 5. 32(5):1161–1165. PMID: 15190967.
Article13. Friedman WA. Resident duty hours in American neurosurgery. Neurosurgery. 2004; 4. 54(4):925–931. discussion 931-3. PMID: 15046659.
Article14. Inaba K, Recinos G, Teixeira PG, Barmparas G, Talving P, Salim A, et al. Complications and death at the start of the new academic year: is there a July phenomenon? J Trauma. 2010; 1. 68(1):19–22. PMID: 20065752.
Article15. Kestle JR, Cochrane DD, Drake JM. Shunt insertion in the summer: is it safe? J Neurosurg. 2006; 9. 105(3 Suppl):165–168. PMID: 16970227.
Article16. Kowalski RG, Claassen J, Kreiter KT, Bates JE, Ostapkovich ND, Connolly ES, et al. Initial misdiagnosis and outcome after subarachnoid hemorrhage. JAMA. 2004; 2. 291(7):866–869. PMID: 14970066.
Article17. Kraus JJ, Metzler MD, Coplin WM. Critical care issues in stroke and subarachnoid hemorrhage. Neurol Res. 2002; 24(Suppl 1):S47–S57. PMID: 12074437.
Article18. Landrigan CP, Rothschild JM, Cronin JW, Kaushal R, Burdick E, Katz JT, et al. Effect of reducing interns' work hours on serious medical errors in intensive care units. N Engl J Med. 2004; 10. 351(18):1838–1848. PMID: 15509817.
Article19. Lockley SW, Cronin JW, Evans EE, Cade BE, Lee CJ, Landrigan CP, et al. Effect of reducing interns' weekly work hours on sleep and attentional failures. N Engl J Med. 2004; 10. 351(18):1829–1837. PMID: 15509816.
Article20. McDonald RJ, Cloft HJ, Kallmes DF. Impact of admission month and hospital teaching status on outcomes in subarachnoid hemorrhage: evidence against the July effect. J neurosurg. 2012; 1. 116(1):157–163. PMID: 21942725.
Article21. Myles TD. Is there an obstetric July phenomenon? Obstet Gynecol. 2003; 11. 102(5 pt 1):1080–1084. PMID: 14672490.
Article22. Pape HC, Pfeifer R. Restricted duty hours for surgeons and impact on residents quality of life, education and patient care: a literature review. Patient Saf Surg. 2009; 2. 3(1):3. PMID: 19232105.
Article23. Phillips DP, Barker GE. A July spike in fatal medication errors - a possible effect of new medical residents. J Gen Intern Med. 2010; 8. 25(8):774–779. PMID: 20512532.24. Rich EC, Gifford G, Luxenberg M, Dowd B. The relationship of house staff experience to the cost and quality of inpatient care. JAMA. 1990; 2. 263(7):953–957. PMID: 2299762.
Article25. Rich ED, Hillson SD, Dowd B, Morris N. Specialty differences in the "July Phenomenon" for Twin Cities teaching hospitals. Med Care. 1993; 1. 31(1):73–83. PMID: 8417272.
Article26. Shulkin DJ. The July phenomenon revisited : are hospital complications associated with new house staff? Am J Med Qual. 1995; Spring. 10(1):14–17. PMID: 7727983.27. Smith ER, Bulter WE, Barker FG 2nd. Is there a "July phenomenon" in pediatric neurosurgery at teaching hospitals? J Neurosurg. 2006; 9. 105(3 Suppl):169–176. PMID: 16970228.
Article28. Walling HW, Veremakis C. Ordering errors by first-year residents: evidence of learning from mistakes. Mo Med. 2004; Mar-Apr. 101(2):128–131. PMID: 15119112.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Symptomatic Tarlov Cyst Following Spontaneous Subarachnoid Hemorrhage
- Spontaneous Spinal Subarachnoid Hemorrhage Report of a Case
- Symptomatic Hydrocephalus after Subarachnoid Hemorrhage
- Computerized Tomography Findings Suggesting Non-aneurysmal Spontaneous Subarachnoid Hemorrhage
- Bilateral Internuclear Ophthalmoplegia Following Spontaneous Subarachnoid Hemorrhage