A Randomized Controlled Trial about the Levels of Radiation Exposure Depends on the Use of Collimation C-arm Fluoroscopic-guided Medial Branch Block
- Affiliations
-
- 1Department of Anesthesiology and Pain Medicine, Konkuk University Medical Center, Seoul, Korea. painfree@kuh.ac.kr
- KMID: 1978659
- DOI: http://doi.org/10.3344/kjp.2013.26.2.148
Abstract
- BACKGROUND
C-arm fluoroscope has been widely used to promote more effective pain management; however, unwanted radiation exposure for operators is inevitable. We prospectively investigated the differences in radiation exposure related to collimation in Medial Branch Block (MBB).
METHODS
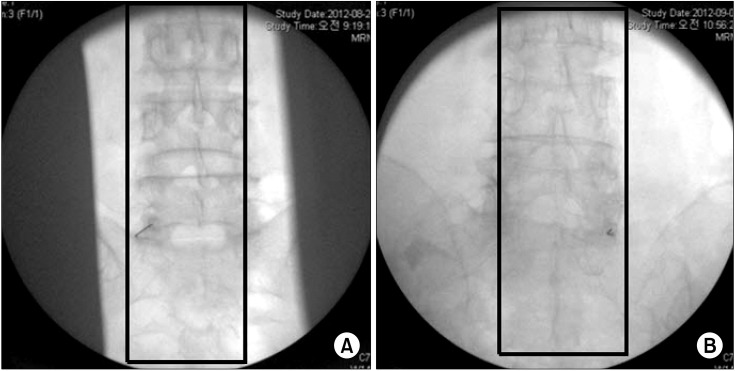
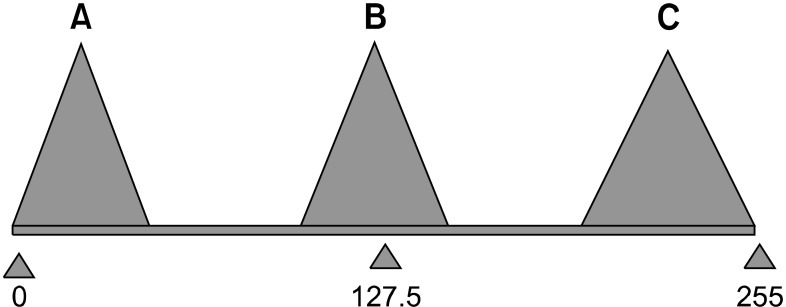
This study was a randomized controlled trial of 62 MBBs at L3, 4 and 5. After the patient was laid in the prone position on the operating table, MBB was conducted and only AP projections of the fluoroscope were used. Based on a concealed random number table, MBB was performed with (collimation group) and without (control group) collimation. The data on the patient's age, height, gender, laterality (right/left), radiation absorbed dose (RAD), exposure time, distance from the center of the field to the operator, and effective dose (ED) at the side of the table and at the operator's chest were collected. The brightness of the fluoroscopic image was evaluated with histogram in Photoshop.
RESULTS
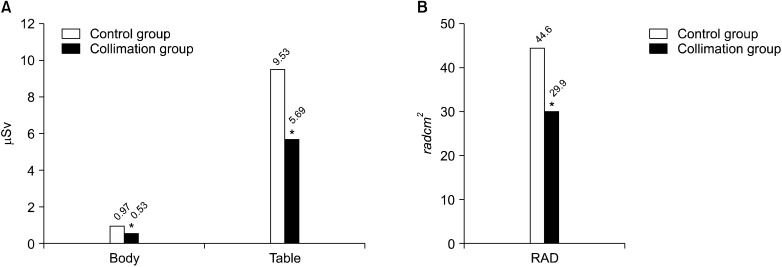
There were no significant differences in age, height, weight, male to female ratio, laterality, time, distance and brightness of fluoroscopic image. The area of the fluoroscopic image with collimation was 67% of the conventional image. The RAD (29.9 +/- 13.0, P = 0.001) and the ED at the left chest of the operators (0.53 +/- 0.71, P = 0.042) and beside the table (5.69 +/- 4.6, P = 0.025) in collimation group were lower than that of the control group (44.6 +/- 19.0, 0.97 +/- 0.92, and 9.53 +/- 8.16), resepectively.
CONCLUSIONS
Collimation reduced radiation exposure and maintained the image quality. Therefore, the proper use of collimation will be beneficial to both patients and operators.
Figure
Cited by 7 articles
-
Effect of Collimation on Radiation Exposure and Image Quality
Mohamed Amin Ghobadifar, Safar Zarei
Korean J Pain. 2013;26(3):307-308. doi: 10.3344/kjp.2013.26.3.307.Radiation Safety for Pain Physicians: Technique or Equipment
Jae Hang Shim
Korean J Pain. 2014;27(2):101-102. doi: 10.3344/kjp.2014.27.2.101.The Radiation Exposure of Radiographer Related to the Location in C-arm Fluoroscopy-guided Pain Interventions
Young Jae Chang, Ah Na Kim, In Su Oh, Nam Sik Woo, Hae Kyoung Kim, Jae Hun Kim
Korean J Pain. 2014;27(2):162-167. doi: 10.3344/kjp.2014.27.2.162.How Effective Are Radiation Reducing Gloves in C-arm Fluoroscopy-guided Pain Interventions?
Ah Na Kim, Young Jae Chang, Bo Kyung Cheon, Jae Hun Kim
Korean J Pain. 2014;27(2):145-151. doi: 10.3344/kjp.2014.27.2.145.The radiation safety education and the pain physicians' efforts to reduce radiation exposure
Tae Hee Kim, Seung Wan Hong, Nam Sik Woo, Hae Kyoung Kim, Jae Hun Kim
Korean J Pain. 2017;30(2):104-115. doi: 10.3344/kjp.2017.30.2.104.Radiation safety: a focus on lead aprons and thyroid shields in interventional pain management
Bo Kyung Cheon, Cho Long Kim, Ka Ram Kim, Min Hye Kang, Jeong Ae Lim, Nam Sik Woo, Ka Young Rhee, Hae Kyoung Kim, Jae Hun Kim
Korean J Pain. 2018;31(4):244-252. doi: 10.3344/kjp.2018.31.4.244.Radiation safety for pain physicians: principles and recommendations
Sewon Park, Minjung Kim, Jae Hun Kim
Korean J Pain. 2022;35(2):129-139. doi: 10.3344/kjp.2022.35.2.129.
Reference
-
1. Fink GE. Radiation safety in fluoroscopy for neuraxial injections. AANA J. 2009; 77:265–269. PMID: 19731844.2. Singer G. Occupational radiation exposure to the surgeon. J Am Acad Orthop Surg. 2005; 13:69–76. PMID: 15712984.
Article3. Miller DL, Vañó E, Bartal G, Balter S, Dixon R, Padovani R, et al. Occupational radiation protection in interventional radiology: a joint guideline of the Cardiovascular and Interventional Radiology Society of Europe and the Society of Interventional Radiology. J Vasc Interv Radiol. 2010; 21:607–615. PMID: 20430294.
Article4. Le Heron J, Padovani R, Smith I, Czarwinski R. Radiation protection of medical staff. Eur J Radiol. 2010; 76:20–23. PMID: 20656429.
Article5. Killewich LA, Singleton TA. Governmental regulations and radiation exposure. J Vasc Surg. 2011; 53:44S–46S. PMID: 20875710.
Article6. Park PE, Park JM, Kang JE, Cho JH, Cho SJ, Kim JH, et al. Radiation safety and education in the applicants of the final test for the expert of pain medicine. Korean J Pain. 2012; 25:16–21. PMID: 22259711.
Article7. Botwin KP, Freeman ED, Gruber RD, Torres-Rames FM, Bouchtas CG, Sanelli JT, et al. Radiation exposure to the physician performing fluoroscopically guided caudal epidural steroid injections. Pain Physician. 2001; 4:343–348. PMID: 16902680.8. Jeong WK. Radiation exposure and its reduction in the fluoroscopic examination and fluoroscopy-guided interventional radiology. J Korean Med Assoc. 2011; 54:1269–1276.
Article9. Poletti JL, McLean D. The effect of source to image-receptor distance on effective dose for some common X-ray projections. Br J Radiol. 2005; 78:810–815. PMID: 16110102.
Article10. Cho JH, Kim JY, Kang JE, Park PE, Kim JH, Lim JA, et al. A study to compare the radiation absorbed dose of the C-arm fluoroscopic modes. Korean J Pain. 2011; 24:199–204. PMID: 22220241.
Article11. Powys R, Robinson J, Kench PL, Ryan J, Brennan PC. Strict X-ray beam collimation for facial bones examination can increase lens exposure. Br J Radiol. 2012; 85:e497–e505. PMID: 22374279.
Article12. Rathmell JP. Rathmell JP, editor. Radiation safety. Atlas of image-guided intervention in regional anesthesia and pain medicine. 2006. Philadelphia: Lippincott Williams & Wilkins;p. 8–15.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Ultrasound Guided Therapeutic Medial Branch Block for the Facet Joint Pain
- Radiation safety for pain physicians: principles and recommendations
- Ultrasound Guided Nerve Block at Vertebra and Lower Extremity
- Radiation exposure and its reduction in the fluoroscopic examination and fluoroscopy-guided interventional radiology
- Radiation Exposure of the Hand and Chest during C-arm Fluoroscopy-Guided Procedures