Tuberc Respir Dis.
2006 Sep;61(3):294-298. 10.4046/trd.2006.61.3.294.
Diffuse Nodular Interstitial Infiltrations with Bilateral Hilar Lymphadenopathy
- Affiliations
-
- 1Department of Internal Medicine, College of Medicine, The Catholic University of Korea, Seoul, Korea. chihongk@yahoo.co.kr
- KMID: 1970271
- DOI: http://doi.org/10.4046/trd.2006.61.3.294
Abstract
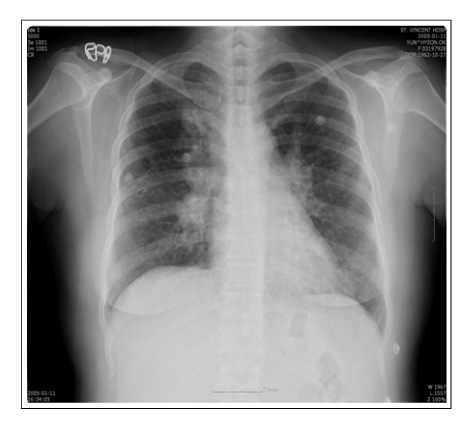
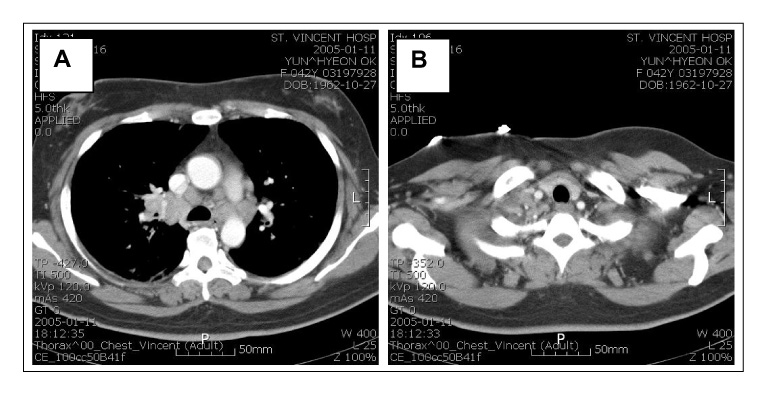
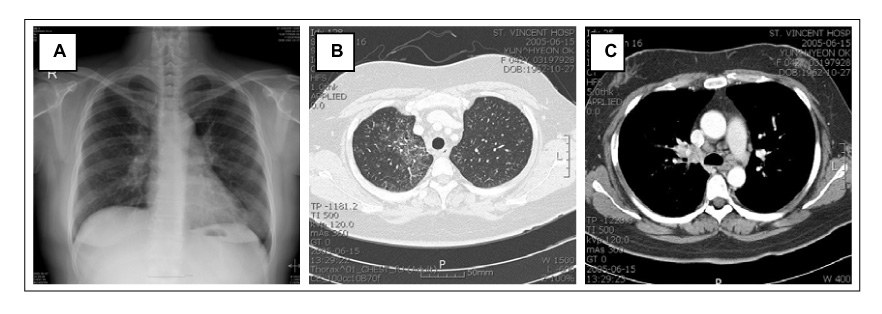
- Lymphocytic interstitial pneumonia(LIP) is an uncommon condition in which the alveolar septa and extra-alveolar interstitial space are markedly expanded by small lymphocytes, plasma cells and histiocytes. Chest radiographs generally show nonspecific patterns with the most common pattern showing bibasilar reticular or reticulonodular infiltrates. Hilar or mediastinal lymphadenopathy and pleural effusions are usually absent. We encountered a 42-year-old female patient who was admitted to hospital because of exertional dyspnea and palpitation. The chest X-ray showed an enlarged bilateral hilar shadow and diffusely increased bronchovascular markings in both lung fields. The chest CT showed diffuse nodular infiltrations with mild septal thickening and combined patchy ground glass opacity in both lungs, and conglomerated mediastinal and bilateral hilar lymphadenopathy. A diagnosis of LIP was made from the tissue pathology taken by a thoracoscopic lung biopsy. The patient showed clinical and radiographic improvement after 3 months of treatment with prednisolone. We report a case of LIP presenting as diffuse nodular interstitial infiltrations with multiple mediastinal and bilateral hilar lymphadenopathy.
Keyword
MeSH Terms
Figure
Reference
-
1. Heitzman ER, Markarian B, Delise CT. Lymphoproliferative disorders of the thorax. Semin Roentgenol. 1975. 10:73–81.2. Nicholson AG. Lymphocytic interstitial pneumonia and other lymphoproliferative disorders in the lung. Semin Respir Crit Care Med. 2001. 22:409–422.3. Liebow AA, Carrington CB. Diffuse pulmonary lymphoreticular infiltrations associated with dysproteinemia. Med Clin North Am. 1973. 57:809–843.4. Teirstein AS, Rosen MJ. Lymphocytic interstitial pneumonia. Clin Chest Med. 1988. 9:467–471.5. Itescu S, Brancato LJ, Boxbaum J, Gregersen PK, Rizk CC, Croxson TS, et al. A diffuse infiltrative CD8 lymphocytosis syndrome in human immunodeficiency virus infection: ahost immune response associated with HLA-DR5. Ann Intern Med. 1990. 112:3–10.6. Alkhayer M, McCann BG, Harrison BD. Lymphocytic interstitial pneumonitis in association with SjÖgren's syndrome. Br J Dis Chest. 1988. 82:305–309.7. Yum MN, Ziegler JR, Walker PD, Ridolfo AS, Brashear RE. Pseudolymphoma of the lung in a patient with systemic lupus erythematosus. Am J Med. 1979. 66:72–76.8. Montes M, Tomasi TB Jr, Noehren TH, Culver GJ. Lymphoid interstitial pneumonia with monoclonal gammopathy. Am Rev Respir Dis. 1968. 98:277–280.9. Jung HJ, Cho ER, Shim JJ, In KH, Yu SH, Kang KH, et al. A case of lymphocytic interstitial pneumonitis. Tuberc Respir Dis. 1993. 40:602–609.10. Bragg DG, Chor PJ, Murray KA, Kjeldsberg CR. Lymphoproliferative disorders of the lung: histopathology, clinical manifestations, and imaging features. AJR Am J Roentgenol. 1994. 163:273–281.11. Strimlan CV, Rosenow EC 3rd, Weiland LH, Brown LR. Lymphocytic interstitial pneumonitis: review of 13 cases. Ann Intern Med. 1978. 88:616–621.12. Fishman AP, Elias JA, Fishman JA, Grippi MA, Kaiser LR, Senior RM. Fishman's pulmonary diseases and disorders. 1998. 3rd ed. New York: McGraw-Hill, Inc;1862–1863.13. Jonkoh T, Ichikado K, Akira M, Honda O, Tomiyama N, Mihara N, et al. Lymphocytic interstitial pneumonia: follow-up CT findings in 14 patients. J Thorac Imaging. 2000. 15:162–167.14. Suh YA, Kim SI, Kim DH, Kwak JY, Lee JC, Baek HJ, et al. A case of lymphocytic interstitial pneumonia. Tuberc Respir Dis. 2001. 51:390–394.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Primary Splenic Lymphoma with Splenic Hilar Lymphadenopathy
- Pulmonary manifestations of tsutsugamushi disease
- Primary T-cell Lymphoma of the Lung Presenting with Bilateral Hilar Lymphadenopathies and Diffuse Pulmonary Infiltration
- Thoracic manifestations of sarcoidosis: CT findings
- HRCT Finding of Pulmonary Cryptococcosis in Immune Competent Patients