J Cerebrovasc Endovasc Neurosurg.
2014 Sep;16(3):216-224. 10.7461/jcen.2014.16.3.216.
Clinico-radiological Characteristics of Spontaneous Basal Ganglia Hemorrhage, According to Regional Classification
- Affiliations
-
- 1Department of Neurosurgery, Gangnam Severance Hospital, Yonsei University College of Medicine Seoul, Korea. ybkim69@yuhs.ac
- KMID: 1963159
- DOI: http://doi.org/10.7461/jcen.2014.16.3.216
Abstract
OBJECTIVE
The clinico-radiologic features of the spontaneous basal ganglia hemorrhage (BGH) may often differ one from another, according to its regional location. Therefore, we attempted to classify the BGH into regional subgroups, and to extrapolate the distinct characteristics of each group of BGH.
MATERIALS AND METHODS
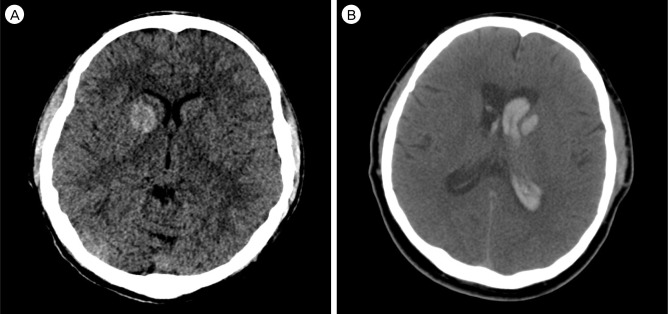
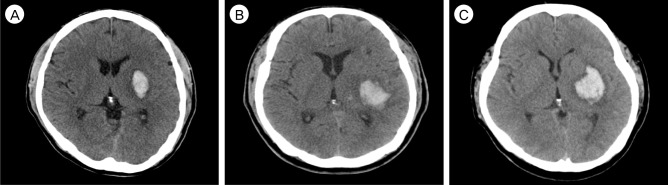
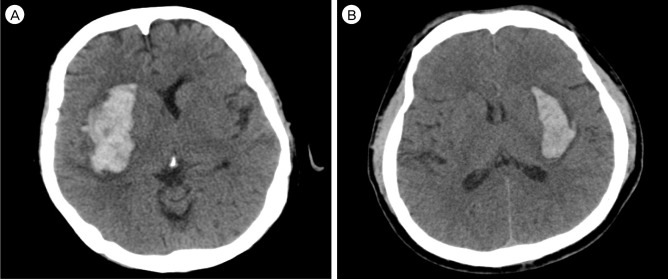
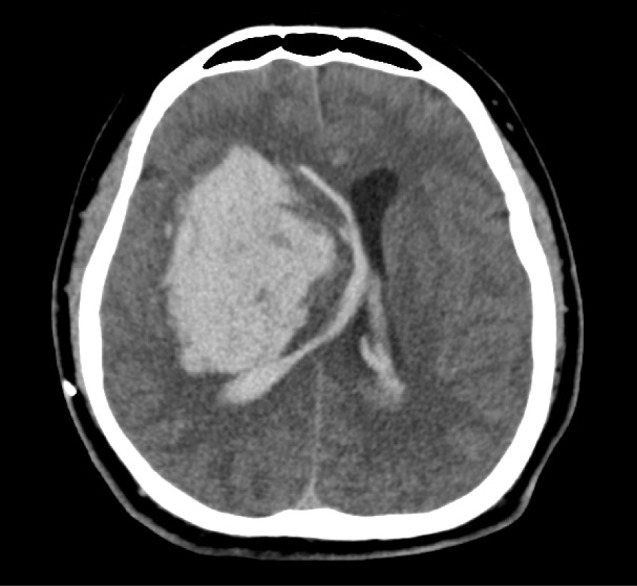
A total of 103 BGHs were analyzed by retrospective review of medical records. BGH was classified according to four subgroups; anterior BGH; posterior BGH; lateral BGH; massive BGH.
RESULTS
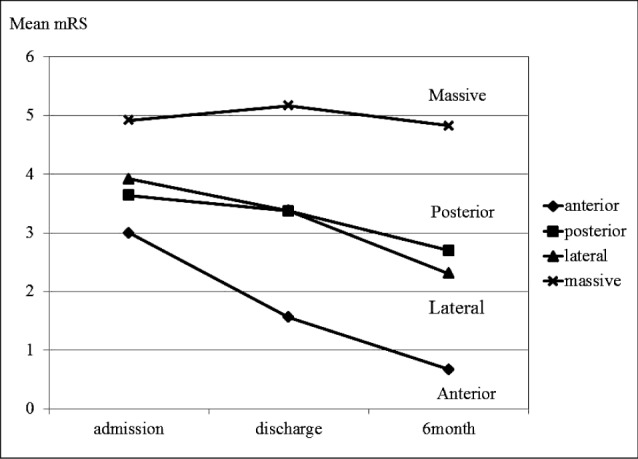
The most common BGH was the posterior BGH (56, 54.4%), followed by the lateral BGH (26, 25.2%), the massive BGH (12, 11.7%), and the anterior BGH (9, 8.7%). The shape of hemorrhage tended to be round in anterior, irregular in posterior, and ovoid in lateral BGH. A layered density of hematoma on initial computed tomography showed correlation with hematoma expansion (p = 0.016), which was observed more often in the postero-lateral group of BGH than in the anterior BGH group. Relatively better recovery from the initial insult was observed in the lateral BGH group than in the other regional BGH groups. The proportion of poor outcome (modified Rankin scale 4, 5, 6) was 100% in the massive, 41.1% in the posterior, 34.6% in the lateral, and 0% in the anterior BGH group.
CONCLUSION
We observed that BGH can be grouped according to its regional location and each group may have distinct characteristics. Thus, a more sophisticated clinical strategy tailored to each group of BGHs can be implemented.
Keyword
MeSH Terms
Figure
Reference
-
1. Barras CD, Tress BM, Christensen S, MacGregor L, Collins M, Desmond PM, et al. Density and shape as CT predictors of intracerebral hemorrhage growth. Stroke. 2009; 4. 40(4):1325–1331. PMID: 19286590.
Article2. Batjer HH, Reisch JS, Allen BC, Plaizier LJ, Su CJ. Failure of surgery to improve outcome in hypertensive putaminal hemorrhage. A prospective randomized trial. Arch Neurol. 1990; 10. 47(10):1103–1106. PMID: 2222242.3. Benes L, Nimsky C. Management of supratentorial intracerebral hemorrhage-still a controversy? World Neurosurg. 2012; 1. 77(1):55–56. PMID: 22154149.
Article4. Chung CS, Caplan LR, Yamamoto Y, Chang HM, Lee SJ, Song HJ, et al. Striatocapsular haemorrhage. Brain. 2000; 9. 123(Pt 9):1850–1862. PMID: 10960049.
Article5. Dennis MS. Outcome after brain haemorrhage. Cerebrovasc Dis. 2003; 16(Suppl 1):9–13. PMID: 12698013.
Article6. Flaherty ML, Haverbusch M, Sekar P, Kissela B, Kleindorfer D, Moomaw CJ, et al. Long-term mortality after intracerebral hemorrhage. Neurology. 2006; 4. 66(8):1182–1186. PMID: 16636234.
Article7. Ghika JA, Bogousslavsky J, Regli F. Deep perforators from the carotid system. Template of the vascular territories. Arch Neurol. 1990; 10. 47(10):1097–1100. PMID: 2222241.8. Hansen BM, Nilsson OG, Anderson H, Norrving B, Saveland H, Lindgren A. Long term (13 years) prognosis after primary intracerebral haemorrhage: a prospective population based study of long term mortality, prognostic factors and causes of death. J Neurol Neurosurg Psychiatry. 2013; 10. 84(10):1150–1155. PMID: 23715913.
Article9. Kazui S, Naritomi H, Yamamoto H, Sawada T, Yamaguchi T. Enlargement of spontaneous intracerebral hemorrhage. Incidence and time course. Stroke. 1996; 10. 27(10):1783–1787. PMID: 8841330.10. Kothari RU, Brott T, Broderick JP, Barsan WG, Sauerbeck LR, Zuccarello M, et al. The ABCs of measuring intracerebral hemorrhage volumes. Stroke. 1996; 8. 27(8):1304–1305. PMID: 8711791.
Article11. Kumral E, Evyapan D, Balkir K. Acute caudate vascular lesions. Stroke. 1999; 1. 30(1):100–108. PMID: 9880396.
Article12. Mendelow AD, Gregson BA, Fernandes HM, Murray GD, Teasdale GM, Hope DT, et al. Early surgery versus initial conservative treatment in patients with spontaneous supratentorial intracerebral haematomas in the international surgical trial in intracerebral haemorrhage (STICH): a randomised trial. Lancet. 2005; Jan-Feb. 365(9457):387–397. PMID: 15680453.
Article13. Mendelow AD, Gregson BA, Rowan EN, Murray GD, Gholkar A, Mitchell PM, et al. Early surgery versus initial conservative treatment in patients with spontaneous supratentorial lobar intracerebral haematomas (STICH II): a randomised trial. Lancet. 2013; 8. 03. 382(9890):397–408. PMID: 23726393.
Article14. Middleton FA, Strick PL. Basal ganglia output and cognition: evidence from anatomical, behavioral, and clinical studies. Brain Cogn. 2000; 3. 42(2):183–200. PMID: 10744919.
Article15. Nagaratnam N, Saravanja D, Chiu K, Jamieson G. Putaminal hemorrhage and outcome. Neurorehabil Neural Repair. 2001; 15(1):51–56. PMID: 11527279.
Article16. Qureshi AI, Tuhrim S, Broderick JP, Batjer HH, Hondo H, Hanley DF. Spontaneous intracerebral hemorrhage. N Engl J Med. 2001; 5. 344(19):1450–1460. PMID: 11346811.
Article17. Talacchi A, Ricci UM, Caramia G, Massimo G. Basal ganglia haemorrhages: efficacy and limits of different surgical strategies. Br J Neurosurg. 2011; 4. 25(2):235–242. PMID: 21158512.
Article18. van Asch CJ, Luitse MJ, Rinkel GJ, van der Tweel I, Algra A, Klijn CJ. Incidence, case fatality, and functional outcome of intracerebral haemorrhage over time, according to age, sex, and ethnic origin: a systematic review and meta-analysis. Lancet Neurol. 2010; 2. 9(2):167–176. PMID: 20056489.
Article