J Korean Foot Ankle Soc.
2015 Mar;19(1):27-31. 10.14193/jkfas.2015.19.1.27.
Intraosseous Calcaneal Lipoma with Subtalar Perforation through Cystic Degeneration: A Case Report
- Affiliations
-
- 1Department of Orthopedic Surgery, Inje University Ilsan Paik Hospital, Goyang, Korea. sjs0506@paik.ac.kr
- 2Department of Surgery, Howard University College of Medicine, Washington, DC, USA.
- 3Department of Pathology, Inje University Ilsan Paik Hospital, Goyang, Korea.
- KMID: 1958702
- DOI: http://doi.org/10.14193/jkfas.2015.19.1.27
Abstract
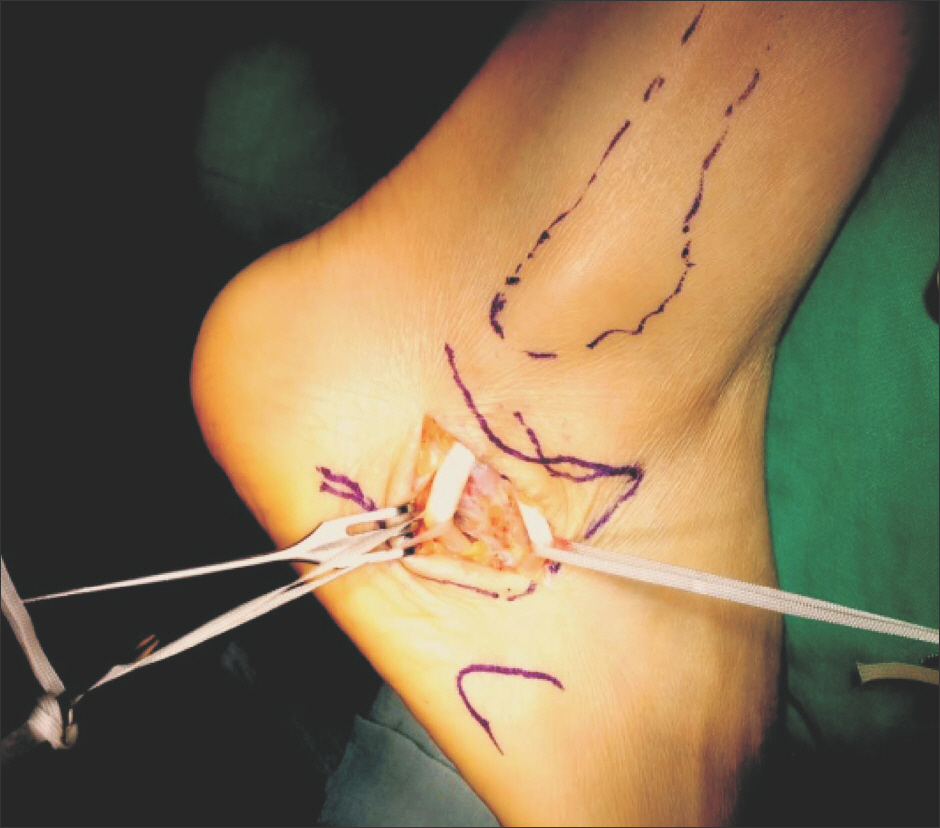
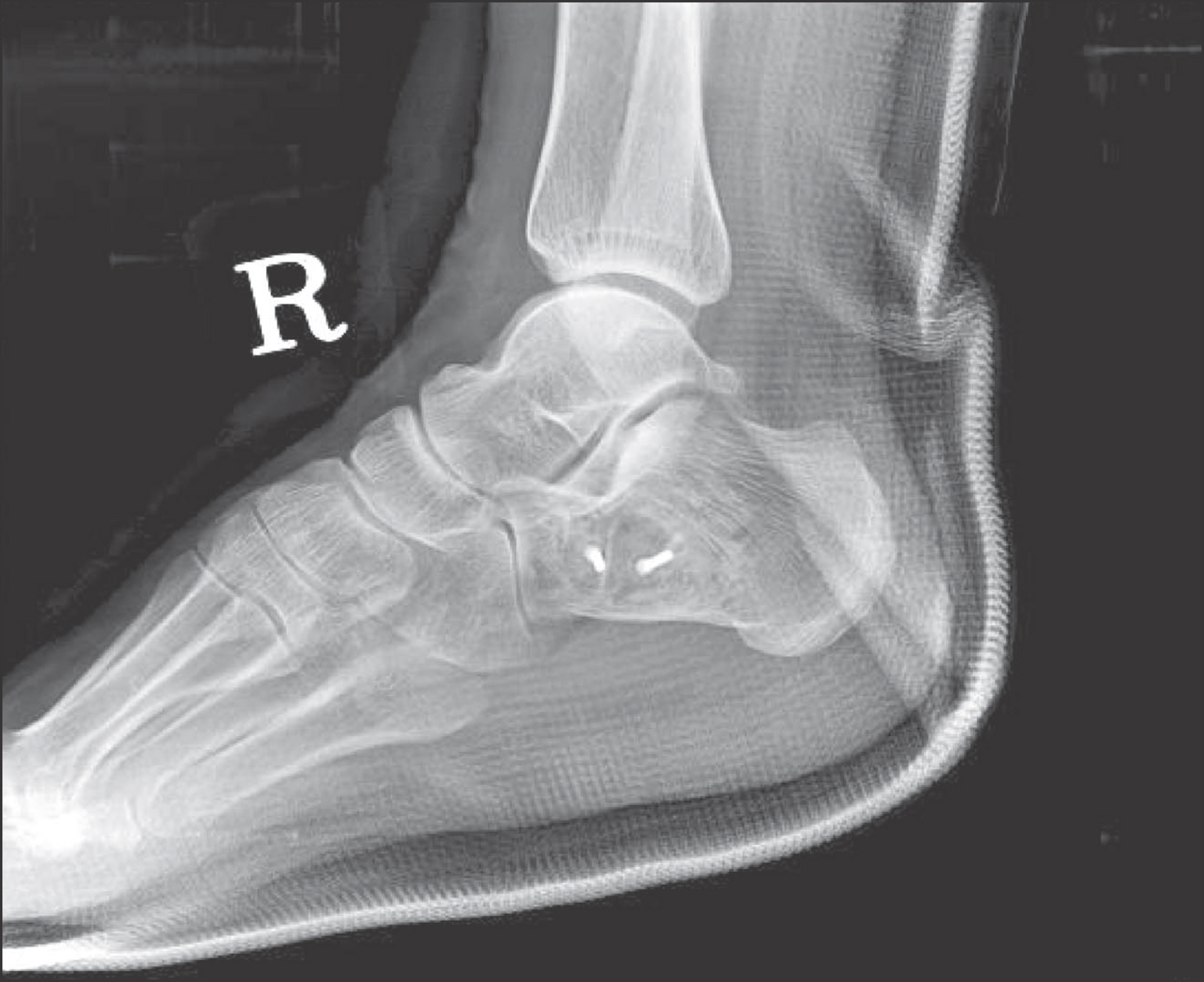
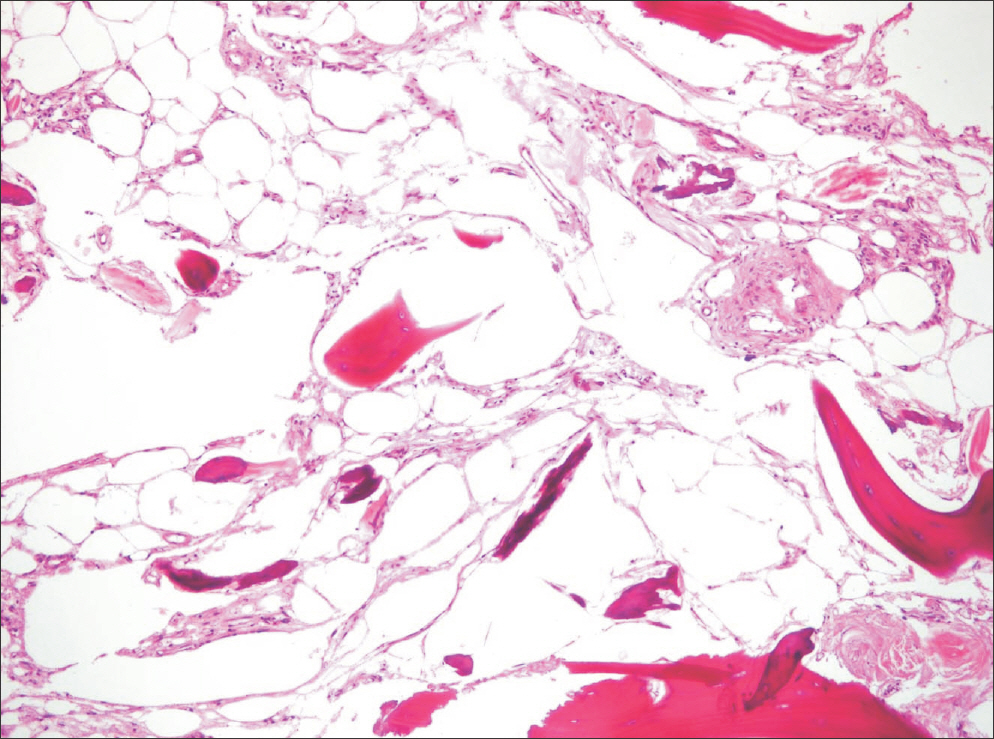
- Intraosseous lipoma is a benign tumor that originates from proliferating mature lipocytes. It often occurs in the metaphysis of long bones of the lower extremity, and also in the calcaneus, humerus, mandible, sacrum, and rib bones. Frequently, it involutes spontaneously through a process of infarction, calcification, and cyst formation. It can either present as pain, or be asymptomatic and only discovered through an incidental radiological finding. In our case, the patient presented with heel pain. Intraoperatively, it was found that the intraosseous cavity was filled with fat along with an adjacent but separate area of cystic degeneration. There was also a cortical perforation at the cystic lesion which was communicating with the subtalar joint. This cortical breach is most likely the cause of diffuse lateral heel pain experienced by our patient, and such a pathological fracture due to intraosseous lipoma has never been reported.
Keyword
MeSH Terms
Figure
Reference
-
1.Bertram C., Popken F., Rütt J. Intraosseous lipoma of the calca-neus. Langenbecks Arch Surg. 2001. 386:313–7.
Article2.Campbell RS., Grainger AJ., Mangham DC., Beggs I., Teh J., Davies AM. Intraosseous lipoma: report of 35 new cases and a review of the literature. Skeletal Radiol. 2003. 32:209–22.
Article3.Chow LT., Lee KC. Intraosseous lipoma. A clinicopathologic study of nine cases. Am J Surg Pathol. 1992. 16:401–10.4.Revenga Martínez M., Bachiller Corral FJ., Rubio García J., Muñoz Beltrán M., Zea Mendoza AC. Cystic lesion of the calcaneus. Intraosseous lipoma. Reumatol Clin. 2007. 3:139–42.
Article5.Milgram JW. Intraosseous lipomas. A clinicopathologic study of 66 cases. Clin Orthop Relat Res. 1988. 231:277–302.6.Abrahim-Zadeh R., Klein RM., Leslie D., Norman A. Characteristics of calcaneal bone infarction: an MR imaging investigation. Skeletal Radiol. 1998. 27:321–4.
Article7.Van Linthoudt D., Lagier R. Calcaneal cysts. A radiological and anatomico-pathological study. Acta Orthop Scand. 1978. 49:310–6.8.Blacksin MF., Ende N., Benevenia J. Magnetic resonance imaging of intraosseous lipomas: a radiologic-pathologic correlation. Skeletal Radiol. 1995. 24:37–41.
Article9.Milgram JW. Malignant transformation in bone lipomas. Skeletal Radiol. 1990. 19:347–52.
Article10.Pappas AJ., Haffner KE., Mendicino SS. An intraosseous lipoma of the calcaneus: a case report. J Foot Ankle Surg. 2014. 53:638–42.
Article