J Korean Med Assoc.
2006 Jul;49(7):612-624. 10.5124/jkma.2006.49.7.612.
Use of Office Spirometry in Primary-Care Clinics
- Affiliations
-
- 1Division of Pulmonary-Allergology, Yeungnam University College of Medicine, Korea. ghlee@med.yu.ac.kr
- KMID: 1958260
- DOI: http://doi.org/10.5124/jkma.2006.49.7.612
Abstract
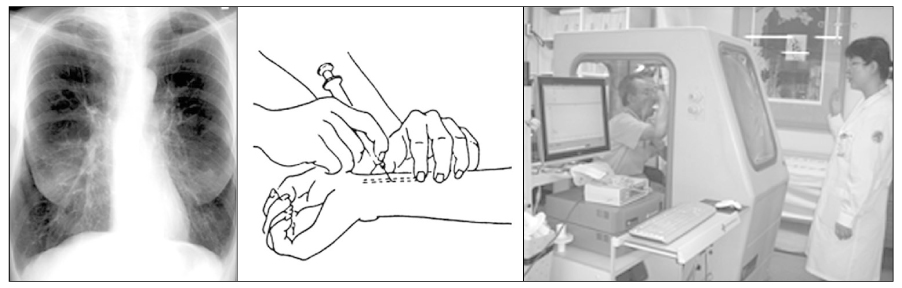
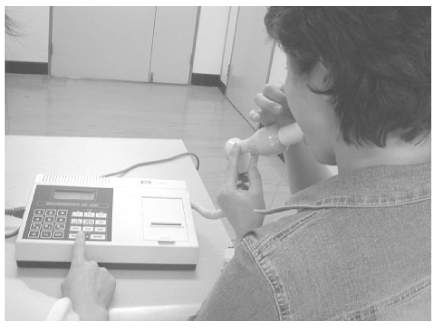
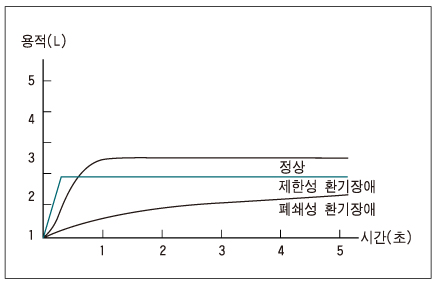
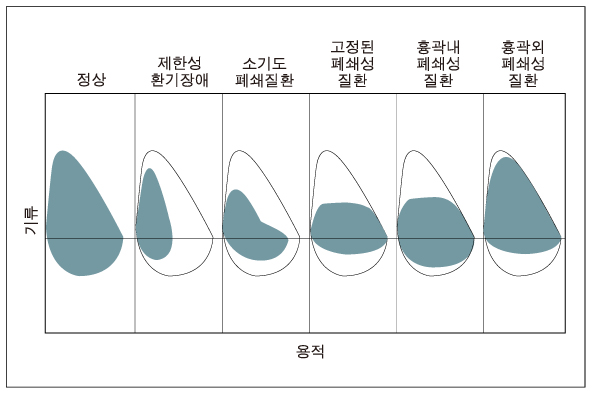
- Early diagnosis and smoking cessation are the only effective ways to stop or delay the progression of chronic obstructive pulmonary disease (COPD). It is true that primarycare physicians rarely use spirometry to establish the diagnosis of COPD in smokers or to detect COPD or asthma in patients with respiratory symptoms or signs. Recently, however, with the advances in the development of electrical devices, a new category of spirometry, "office spirometry", has been introduced. Office spirometry is a simple, safe, and noninvasive test. In addition, it takes only a few minutes for the patient and technician to perform office spirometry, which includes a few breathing maneuvers of a 6-second duration. Primary-care physicians are strongly encouraged to perform an office spirometry test in patients with respiratory symptoms such as chronic cough, sputum, wheezing, dyspnea or in patients over 45 years of age who report smoking cigarettes in order to detect COPD.
MeSH Terms
Figure
Reference
-
1. Enright PL, Hyatt RE. Office Spirometry A Practical Guide to the Selection and Use of Spirometers. 1896. Philadelphia: Lea & Febiger.2. Ferguson GT, Enright PL, Buist AS, Higgins MW. Office Spirometry for Lung Health Assessment in Adults: A Consensus Statement From the National Lung Health Education Program. Chest. 2000. 117:1146–1161.
Article3. Miller MR, Hankinson J, Brusasco V, Burgos F, Casaburi R, Wanger J, et al. Standardisation of spirometry. Eur Respir J. 2005. 26:319–338.
Article5. Weinberger SE, Drazen JM. Kasper DL, Braunwald E, Fauci AS, Hauser S, Longo D, Jameson JL, editors. Disturances of Respiratory Function. Harrison's Principles of Internal Medicine. 2005. 16th ed. New York: McGraw-Hill;1498–1501.6. Buffels J, Degryse J, Heyrman MDJ, Decramer M. Office Spirometry Significantly Improves Early Detection of COPD in General Practice. Chest. 2004. 125:1394–1399.
Article7. Dales RE, Vandemheen KL, Clinch J, Aaron SD. Spirometry in the Primary Care Setting. Influence on Clinical Diagnosis and Management of Airflow Obstruction. Chest. 2005. 128:2443–2447.
Article8. Bolton CE, Ionescu AA, Edwards PH, Faulkner TA, Edwards SM, Shale DJ. Attaining a correct diagnosis of COPD in general practice. Respiratory Medicine. 2005. 99:493–500.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The learning characteristics of primary care physicians
- Qualitative Research on Experience of Primary Physicians Operating Their Primary Health Care Centers
- Management of allergic rhinitis in general practitioners
- Patients' Perceived Quality of Family Physicians' Primary Care with or without 'Family Medicine' in the Clinic Name
- Definition and Status of Funtional Primary Clinic in Korea