J Korean Neurosurg Soc.
2014 Aug;56(2):130-134. 10.3340/jkns.2014.56.2.130.
A Groove Technique for Securing an Electrode Connector on the Cranial Bone: Case Analysis of Efficacy
- Affiliations
-
- 1Department of Neurosurgery, Maryknoll Hospital, Busan, Korea. stereomk@naver.comr
- KMID: 1956515
- DOI: http://doi.org/10.3340/jkns.2014.56.2.130
Abstract
OBJECTIVE
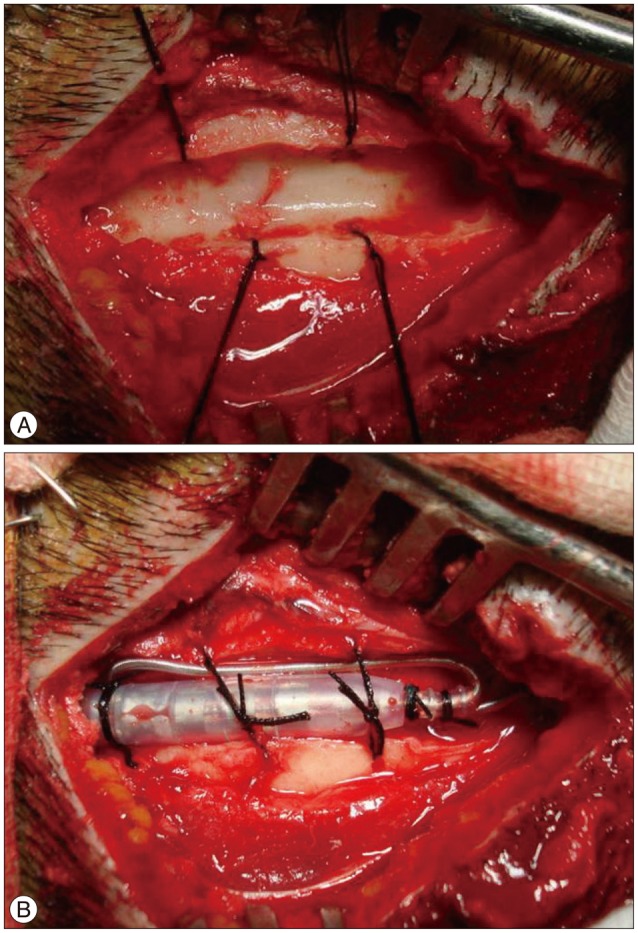
A groove technique for securing an electrode connector was described as an alternative surgical technique in deep brain stimulation (DBS) surgery to avoid electrode connector-related complications, such as skin erosion, infection, and migration.
METHODS
We retrospectively reviewed 109 patients undergoing one of two techniques; the standard technique (52 patients using 104 electrodes) and the groove technique (57 patients using 109 electrodes) for securing the electrode connector in DBS surgery, regardless of patient disease. In the standard percutaneous tunneling technique, the connector was placed on the vertex of the cranial surface. The other technique, so called the groove technique, created a groove (about 4 cm long, 8 mm wide) in the cranial bone at the posterior parietal area. Wound erosion and migration related to the connectors were compared between the two techniques.
RESULTS
The mean follow-up period was 73 months for the standard method and 46 months for the groove technique. Connector-related complications were observed in three patients with the groove technique and in seven patients with the standard technique. Wound erosion at the connector sites per electrode was one (0.9%) with the groove technique and six (5.8%) with the standard technique. This difference was statistically significant. The electrode connector was migrated in two patients with the groove technique and in one patient with the standard technique.
CONCLUSIONS
The groove technique, which involves securing an electrode using a groove in the cranial bone at the posterior parietal area, offers an effective and safe method to avoid electrode connector-related complications during DBS surgery.
Keyword
MeSH Terms
Figure
Reference
-
1. Alim LB, John M, Stephan C, Eric S, Napoleon T, Brigitte P, et al. Subthalamic deep brain stimulation for Parkinson's disease. In : Youmans JR, editor. Neurological Surgery. ed 6. Saunders: Elsevier;2011. 1:p. 944–962.2. Bhatia R, Dalton A, Richards M, Hopkins C, Aziz T, Nandi D. The incidence of deep brain stimulator hardware infection : the effect of change in antibiotic prophylaxis regimen and review of the literature. Br J Neurosurg. 2011; 25:625–631. PMID: 21501065.
Article3. Chou YC, Lin SZ, Hsieh WA, Lin SH, Lee CC, Hsin YL, et al. Surgical and hardware complications in subthalamic nucleus deep brain stimulation. J Clin Neurosci. 2007; 14:643–649. PMID: 17532500.
Article4. Hariz MI. Complications of deep brain stimulation surgery. Mov Disord. 2002; 17(Suppl 3):S162–S166. PMID: 11948772.
Article5. Hu X, Jiang X, Zhou X, Liang J, Wang L, Cao Y, et al. Avoidance and management of surgical and hardware-related complications of deep brain stimulation. Stereotact Funct Neurosurg. 2010; 88:296–303. PMID: 20588081.
Article6. Kim EU, Kim JM, Yoo CJ, Lee U. The procedure of cables insertion in deep brain stimulation surgery. J Korean Soc Stereotact Funct Neurosurg. 2011; 7:37–40.7. Louis AW, Kim JB. Deep brain stimulation in movement disorders : Parkinson's disease, essential tremor, and dystonia. In : Schmidek HH, editor. Operative neurosurgical techniques. ed 6. Saunders: Elsevier;2012. 2:p. 1309–1320.8. Oh MY, Abosch A, Kim SH, Lang AE, Lozano AM. Long-term hardware-related complications of deep brain stimulation. Neurosurgery. 2002; 50:1268–1274. discussion 1274-1276. PMID: 12015845.
Article9. Pahwa R, Lyons KE, Wilkinson SB, Simpson RK Jr, Ondo WG, Tarsy D, et al. Long-term evaluation of deep brain stimulation of the thalamus. J Neurosurg. 2006; 104:506–512. PMID: 16619653.
Article10. Park YS, Kang JH, Kim HY, Kang DW, Chang WS, Kim JP, et al. A combination procedure with double C-shaped skin incision and dual-floor burr hole method to prevent skin erosion on the scalp and reduce postoperative skin complications in deep brain stimulation. Stereotact Funct Neurosurg. 2011; 89:178–184. PMID: 21508657.
Article11. Peña E, Pastor J, Hernando V, Gallego I, Pedrosa M, Carrasco R, et al. Skin erosion over implants in deep brain stimulation patients. Stereotact Funct Neurosurg. 2008; 86:120–126. PMID: 18270483.
Article12. Rezai AR, Kopell BH, Gross RE, Vitek JL, Sharan AD, Limousin P, et al. Deep brain stimulation for Parkinson's disease : surgical issues. Mov Disord. 2006; 21(Suppl 1):S197–S218. PMID: 16810673.13. Rezai AR, Machado AG, Deogaonkar M, Azmi H, Kubu C, Boulis NM. Surgery for movement disorders. Neurosurgery. 62(Suppl 2):2008; 809–838. PMID: 18596424.
Article14. Sierens D, Kutz S, Philitsis JG, Bakay RA. Stereotactic surgery with microelectrode recordings. In : Bakay RA, editor. Movement disorder surgery. New York: Thieme;2009. p. 214–216.15. Sillay KA, Larson PS, Starr PA. Deep brain stimulator hardware-related infections : incidence and management in a large series. Neurosurgery. 2008; 62:360–366. discussion 366-367. PMID: 18382313.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Three-dimensional finite element analysis for the effect of retentive groove design on joint strength of casting connection
- Perineal Groove: A Case Report and Re view of Literature
- Treatment of a lateral incisor anatomically complicated with palatogingival groove
- Removal of Entrapped Pacemaker Electrode: One Case Report
- Contribution of the Dura & the Pericranium in Absorption of Cranial Bone