J Korean Soc Radiol.
2014 May;70(5):335-342. 10.3348/jksr.2014.70.5.335.
Hepatic Angiographic Findings of Ruptured Hepatocellular Carcinoma: "Sentinel Signs" versus Extravasation
- Affiliations
-
- 1Department of Radiology, Kyung Hee University Hospital at Gangdong, Kyung Hee University School of Medicine, Seoul, Korea. namjindan@daum.net
- KMID: 1941777
- DOI: http://doi.org/10.3348/jksr.2014.70.5.335
Abstract
- PURPOSE
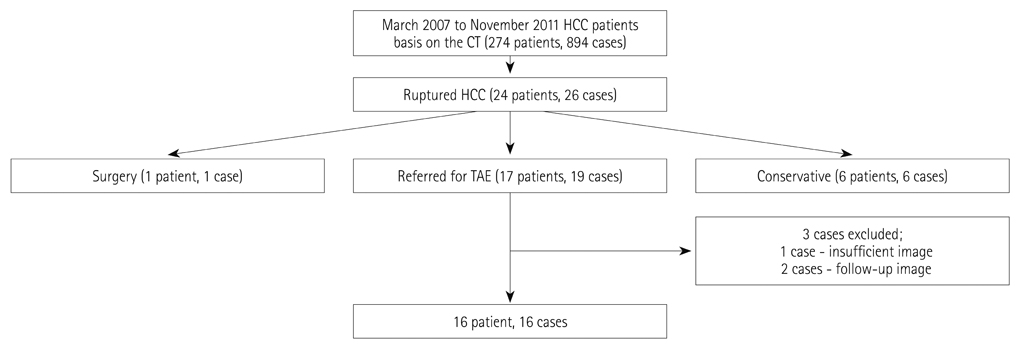
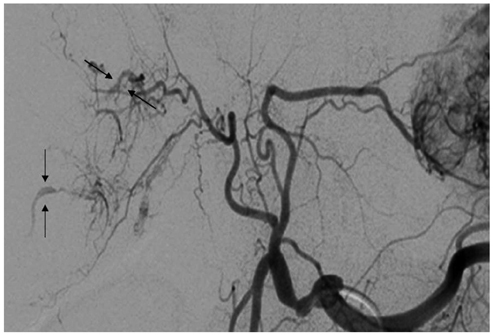
This study retrospectively compared the accuracy of angiographic sentinel signs (sentinel vessels, hypovascular areas, and delayed dots) with extravasation in the diagnosis of ruptured hepatocellular carcinoma (HCC).
MATERIALS AND METHODS
Sixteen patients diagnosed with HCC between March 2007 and November 2011 were evaluated. Among the patients, we identified 32 HCCs (19 ruptured, 13 unruptured), and assessed all HCCs by hepatic angiography with regard to extravasation, sentinel vessels, hypovascular areas, and delayed dots. We compared the sensitivity and specificity of the sentinel signs with those of the extravasation for the diagnosis of a ruptured HCC.
RESULTS
For the angiographic diagnosis of a ruptured HCC, the sensitivity of the sentinel signs (sentinel vessel, 63.2%; hypovascular area, 89.5%; delayed dot, 72.7%) was higher than the sensitivity of extravasation (15.8%). The difference in sensitivity between each sentinel sign and extravasation was statistically significant (sentinel vessel, p = 0.012; hypovascular area, p < 0.001; delayed dot, p = 0.039). The specificity of sentinel signs for the diagnosis of ruptured HCC was not statistically different from the specificity of extravasation.
CONCLUSION
Sentinel signs are more accurate than extravasation for the angiographic diagnosis of a ruptured HCC.
MeSH Terms
Figure
Reference
-
1. Casillas VJ, Amendola MA, Gascue A, Pinnar N, Levi JU, Perez JM. Imaging of nontraumatic hemorrhagic hepatic lesions. Radiographics. 2000; 20:367–378.2. Lubner M, Menias C, Rucker C, Bhalla S, Peterson CM, Wang L, et al. Blood in the belly: CT findings of hemoperitoneum. Radiographics. 2007; 27:109–125.3. Lai EC, Lau WY. Spontaneous rupture of hepatocellular carcinoma: a systematic review. Arch Surg. 2006; 141:191–198.4. Choi BG, Park SH, Byun JY, Jung SE, Choi KH, Han JY. The findings of ruptured hepatocellular carcinoma on helical CT. Br J Radiol. 2001; 74:142–146.5. Miyoshi A, Kitahara K, Kohya N, Noshiro H, Miyazahi K. Outcomes of patients with spontaneous rupture of hepatocellular carcinoma. Hepatogastroenterology. 2011; 58:99–102.6. Al-Mashat FM, Sibiany AM, Kashgari RH, Maimani AA, Al-Radi AO, Balawy IA, et al. Spontaneous rupture of hepatocellular carcinoma. Saudi Med J. 2002; 23:866–870.7. Liu CL, Fan ST, Lo CM, Tso WK, Poon RT, Lam CM, et al. Management of spontaneous rupture of hepatocellular carcinoma: single-center experience. J Clin Oncol. 2001; 19:3725–3732.8. Chen CY, Lin XZ, Shin JS, Lin CY, Leow TC, Chen CY, et al. Spontaneous rupture of hepatocellular carcinoma. A review of 141 Taiwanese cases and comparison with non-rupture cases. J Clin Gastroenterol. 1995; 21:238–242.9. Leung KL, Lau WY, Lai PB, Yiu RY, Meng WC, Leow CK. Spontaneous rupture of hepatocellular carcinoma: conservative management and selective intervention. Arch Surg. 1999; 134:1103–1107.10. Ngan H, Tso WK, Lai CL, Fan ST. The role of hepatic arterial embolization in the treatment of spontaneous rupture of hepatocellular carcinoma. Clin Radiol. 1998; 53:338–341.11. Corr P, Chan M, Lau WY, Metreweli C. The role of hepatic arterial embolization in the management of ruptured hepatocellular carcinoma. Clin Radiol. 1993; 48:163–165.12. Battula N, Madanur M, Priest O, Srinivasan P, O'Grady J, Heneghan MA, et al. Spontaneous rupture of hepatocellular carcinoma: a Western experience. Am J Surg. 2009; 197:164–167.13. Kim HC, Yang DM, Jin W, Park SJ. The various manifestations of ruptured hepatocellular carcinoma: CT imaging findings. Abdom Imaging. 2008; 33:633–642.14. Kim PT, Su JC, Buczkowski AK, Schaeffer DF, Chung SW, Scudamore CH, et al. Computed tomography and angiographic interventional features of ruptured hepatocellular carcinoma: pictorial essay. Can Assoc Radiol J. 2006; 57:159–168.15. Tarantino L, Sordelli I, Calise F, Ripa C, Perrotta M, Sperlongano P. Prognosis of patients with spontaneous rupture of hepatocellular carcinoma in cirrhosis. Updates Surg. 2011; 63:25–30.16. Ong GB, Taw JL. Spontaneous rupture of hepatocellular carcinoma. Br Med J. 1972; 4:146–149.17. Kim PN, Kim IY, Bae WK, Lee BH. Computed tomographic findings of ruptured hepatic malignancy. Gastrointest Radiol. 1991; 16:334–336.18. Hermann RE, David TE. Spontaneous rupture of the liver caused by hepatomas. Surgery. 1973; 74:715–719.19. Zhu LX, Wang GS, Fan ST. Spontaneous rupture of hepatocellular carcinoma. Br J Surg. 1996; 83:602–607.20. Veltchev LM. Spontaneous rupture of hepatocellular carcinoma and hemoperitoneum-management and long term survival. J IMAB. 2009; 15:53–57.21. Chearanai O, Plengvanit U, Asavanich C, Damrongsak D, Sindhvananda K, Boonyapisit S. Spontaneous rupture of primary hepatoma: report of 63 cases with particular reference to the pathogenesis and rationale treatment by hepatic artery ligation. Cancer. 1983; 51:1532–1536.22. Zhu LX, Geng XP, Fan SD. [Mechanism of spontaneous rupture of hepatocellular carcinoma]. Zhonghua Wai Ke Za Zhi. 2004; 42:1036–1039.23. Zhu LX, Meng XL, Fan ST. Elasticity of small artery in patient with spontaneous rupture of hepatocellular carcinoma. Hepatol Res. 2004; 29:13–17.24. Zhu LX, Liu Y, Fan ST. Ultrastructural study of the vascular endothelium of patients with spontaneous rupture of hepatocellular carcinoma. Asian J Surg. 2002; 25:157–162.25. Zhu LX, Geng XP, Fan ST. Spontaneous rupture of hepatocellular carcinoma and vascular injury. Arch Surg. 2001; 136:682–687.26. Zhu LX, Geng XP, Fan ST. Relationship between vascular elasticity and spontaneous rupture of hepatocellular carcinoma. The Chin-Ger J Clin Oncol. 2003; 2:18–22.27. Soyer P, Van Beers B, Goffette P, Zeitoun G, Pringot J, Leves-que M. [The role of embolization and chemo-embolization in the emergency treatment of hemoperitoneum caused by spontaneous rupture of hepatocellular carcinoma]. Gastroenterol Clin Biol. 1993; 17:643–648.28. Shibata T, Maetani Y, Ametani F, Kubo T, Itoh K, Konishi J. Efficacy of nonsurgical treatments for hepatocellular carcinoma in the caudate lobe. Cardiovasc Intervent Radiol. 2002; 25:186–192.29. Miyayama S, Yamashiro M, Hashimoto M, Hashimoto N, Ikuno M, Okumura K, et al. Identification of small hepatocellular carcinoma and tumor-feeding branches with cone-beam CT guidance technology during transcatheter arterial chemoembolization. J Vasc Interv Radiol. 2013; 24:501–508.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Angiographic Extravasation
- Repeat Resection for Intrahepatic and Omental Recurrence of Ruptured Hepatocelluar Carcinoma after the Initial Surgery
- Angiographic findings of hepatocellular carcinoma
- CT findings in ruptured hepatocellular carcinoma
- A case of spontaneous hepatic rupture in a patient with primary hepatocellular carcinoma during the puerperium