J Korean Soc Spine Surg.
2007 Jun;14(2):79-86. 10.4184/jkss.2007.14.2.79.
Minimally Invasive Microscopic Decompression with Tubular Retractor System in Lumbar Spinal Stenosis: Results Comparing with Open Microscopic Decompression
- Affiliations
-
- 1Department of Orthopedic Surgery, Kosin University, Gospel Hospital, Busan, Korea. drjang@hanafos.com
- KMID: 1941659
- DOI: http://doi.org/10.4184/jkss.2007.14.2.79
Abstract
-
PURPOSE: To compare the two methods of decompression using a microscope with a tubular retractor system and open microscopic decompression in lumbar spinal stenosis.
MATERIALS AND METHODS
The records of patients that had undergone decompression from May 2000 to April 2005 were reviewed. The average follow-up period was 29 months (4~60 months). The duration of hospital stay, estimated blood loss, relief of pain, and operating time were reviewed retrospectively. Analysis was conducted by telephone interview and chart review (McNab's criteria). Pre- and post-operative Visual Analogue Scale (VAS) scores and JOA scores were also evaluated.
RESULTS
Of the total 53 patients, open microscopic decompression was performed on 27 patients, and 26 patients received surgery using microscopic decompression with tubular retractors. There were no patients who had serious complications such as infection or nerve root injury in either of the groups. The average estimated blood loss was 205 cc for the open microscopic decompression group versus 120 cc in the minimally invasive microscopic decompression (MIMD) group (p=0.019). The mean operating time was 2.5 hours in the open microscopic decompression group and 2.2 hours in the MIMD group (p=0.048). As shown by the clinical results, good or excellent results were shown by the McNab's criteria after operation, 85.1% for the open microscopic decompression group and 94.7% for the MIMD group, respectively. The JOA score improved after surgery, with average scores of 14.5 to 24.5 in the open microscopic decompression group, and 15.9 to 25.6 in the MIMD group. The VAS score was reduced after surgery, with an average score of 8.0 to 3.7 in the open microscopic decompression group, and 8.3 to 2.6 in the MIMD group.
CONCLUSION
In terms of blood loss, the MIMD group showed significantly better results than the open microscopic decompression group. The clinical results showed no statistically significant difference between the two groups.
Keyword
MeSH Terms
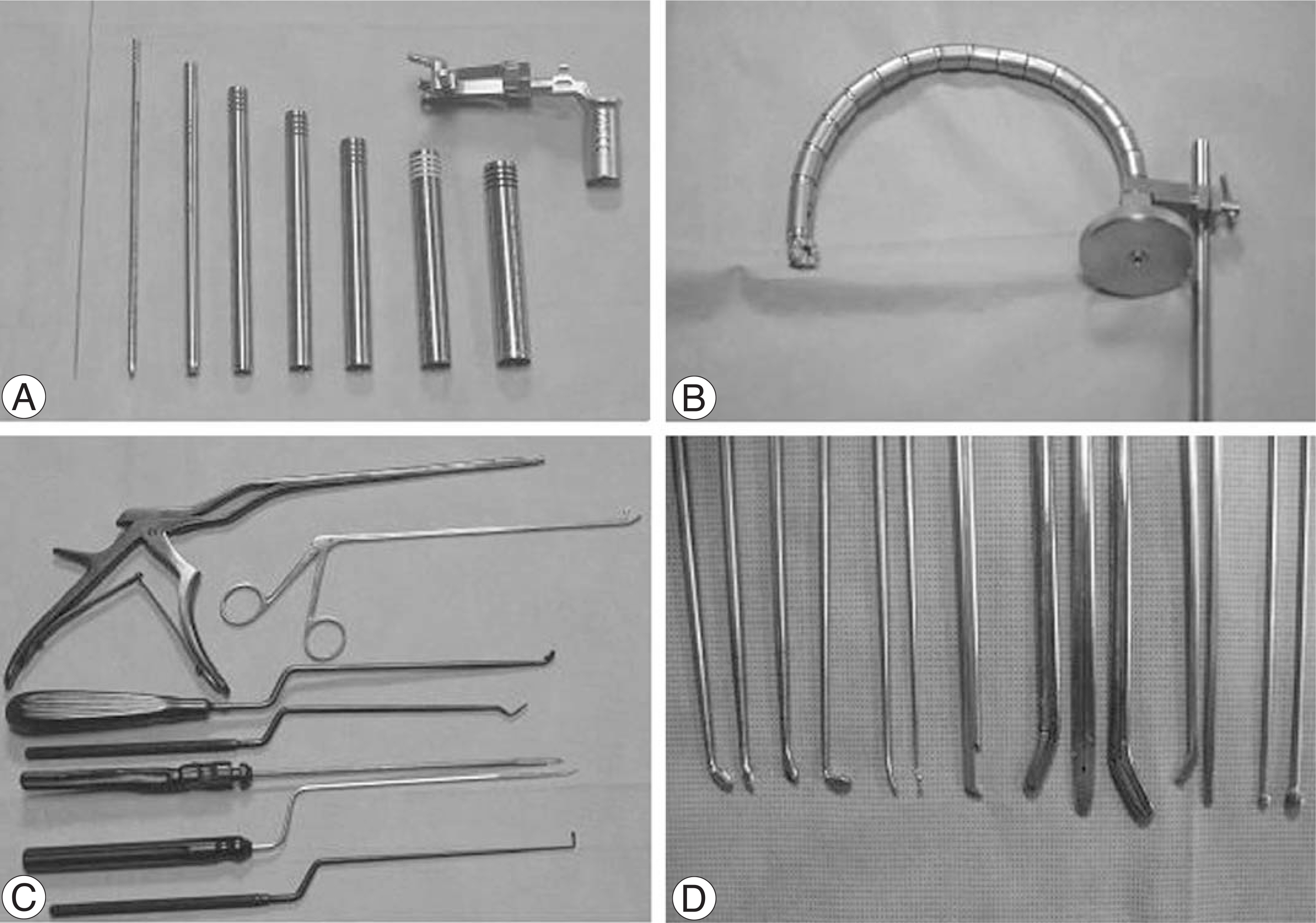
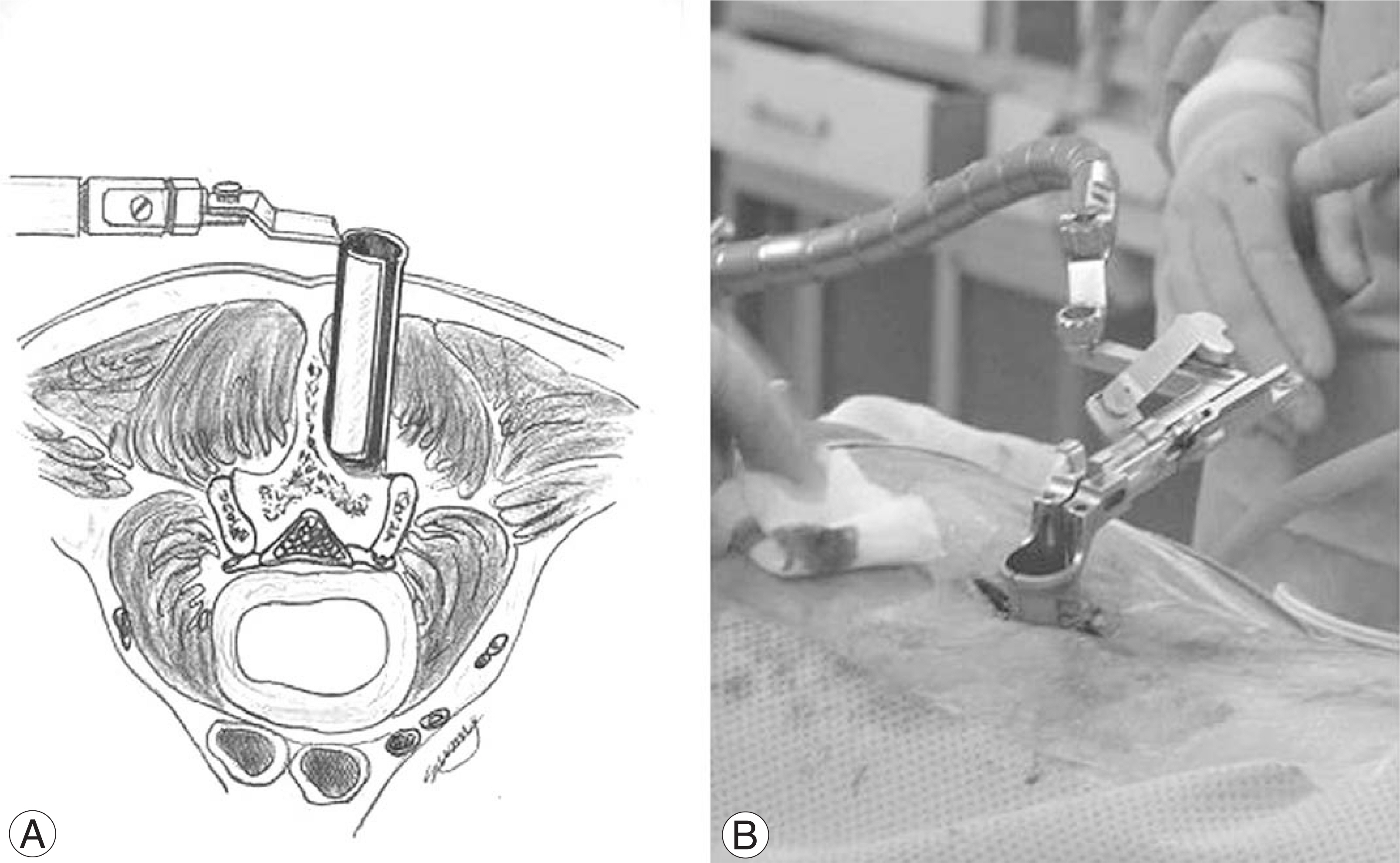
Figure
Reference
-
1). Mimran RI, Henn JS. Minimally invasive lumbar decompression. Oper Tech Neurosurg. 2005; 7:56–63.
Article2). Song HH, Shim DM, Kim DC, Kim TK, Shin HS. Selective microscopic decompression for multilevel lumbar spinal stenosis. J Korean Soc Spine Surg. 2000; 7:552–557.3). Lee CS, Chung SS, Chung KH, Oh SK. Bilateral microscopic laminotomy for lumbar spinal stenosis. J Korean Soc Spine Surg. 2004; 11:99–103.
Article4). Eule JM, Breeze R, Kindt GW. Bilateral partial laminectomy: a treatment for lumbar spinal stenosis and midline disc herniation. Surg Neurol. 1999; 52:329–338.
Article5). Macnab I. Negative disc exploration. J Bone Joint Surg Am. 1971; 53:891–903.
Article6). Posner I, White AA, Edwards WT, Hayes WC. A biomechanical analysis of clinical stability of the lumbar lumbosacral spine. Spine. 1982; 7:374.7). Kim WJ, Kang JW, Park JG, et al. .:. Surgical outcome of degenerative lumbar spinal stenosis in patients over 70 years old- a comparative analysis according to surgical method. J Korean Soc Spine Surg. 2005; 12:101–105.
Article8). Choi H, Kim H, Cho HL, Shin SH, Ko YC, Kim YD. Treatment of degenerative lumbar stenosis with minimal decompression. J Korean Soc Spine Surg. 2003; 10:154–162.
Article9). Jaikumar S, Kim DH, Kam AC. History of minimally invasive spine surgery. J Neurosurg. 2002; 51:1–14.
Article10). Pool JL. Myeloscopy: Intraspinal endoscopy. Surgery. 1942; 11:169–182.
Article11). Malis JL. Technical contributions of Leonard I. Malis Mt Sinai J Med. 1977; 64:172–181.12). Yasargil MG. Microsurgical operation of herniated lumber disc. Adv Neurosurg. 1977; 4:81.13). Caspar W. A new surgical procedure for lumber disc herniation causing less tissue through a microsurgical approach. Adv Neurosurg. 1977; 4:74–80.14). Kambin P, Gellman H. Percutaneous lateral discectomy of the lumbar spine: A preliminary report. Clin Orthop. 1983; 174:127–132.15). Smith MM, Foley KT. Microendoscopic discectomy (MED). J Neurosurg. 1998; 43:702.16). Kim JD. Micro endoscopic disectomy (MED). J Korean Soc Spine Surg. 2000; 7:298–302.17). Grab D, Hunke T, Dvorak J. Degenerative lumbar spinal stenosis. Decompression with and without arthrodesis. J Bone Joint Surg Am. 1995; 75:1036–1041.18). Spivak JM. Current Concept of review-degenerative lumbar spinal stenosis. J Bone Joint Surg Am. 1998; 80:1053–1066.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Clinical Applications of the Tubular Retractor on Spinal Disorders
- Biportal Endoscopic Transforaminal Lumbar Interbody Fusion with Arthroscopy
- Unilateral Laminectomy and Bilateral Decompression for Lumbar Spinal Stenosis with Microscope and Tubular Retractor System
- Usefulness of Minimally Invasive Posterior Foraminotomy using Tubular Retractor for Lumbar Spinal Stenosis with Foraminal Stenosis
- Biportal Percutaneous Endoscopic Spinal Surgery for Lumbar Spinal Stenosis