Neurointervention.
2014 Feb;9(1):32-38. 10.5469/neuroint.2014.9.1.32.
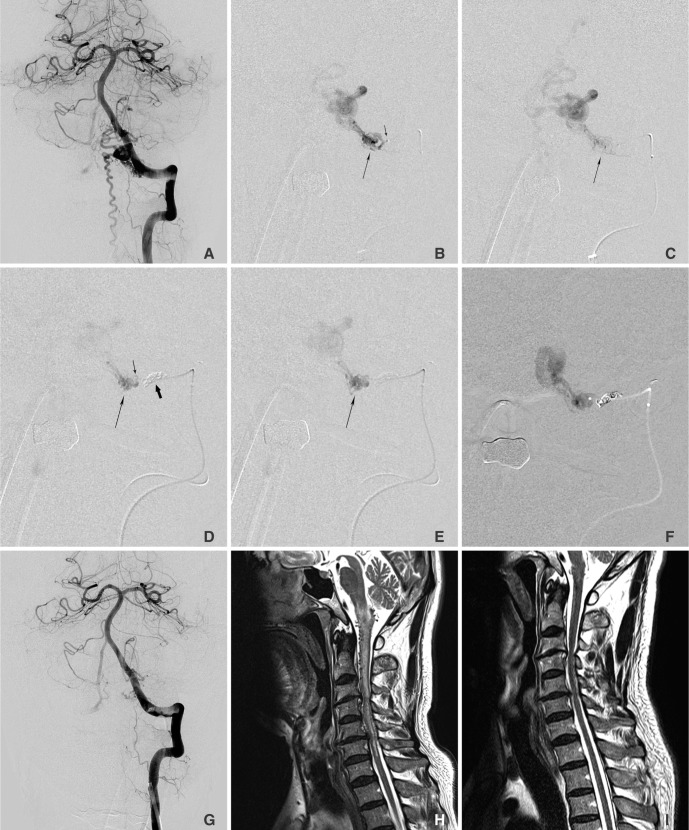
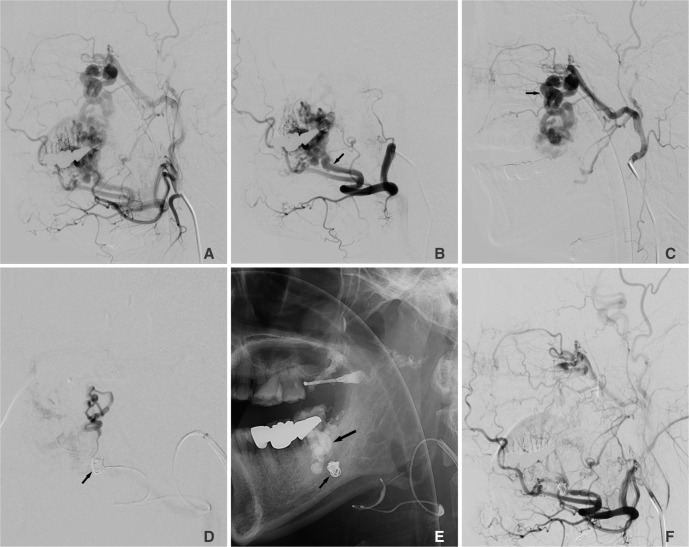
Two Microcatheter Technique for Embolization of Arteriovenous Fistula with Liquid Embolic Agent
- Affiliations
-
- 1Department of Radiology and Research Institute of Radiology, University of Ulsan, College of Medicine, Asan Medical Center, Seoul, Korea. dcsuh@amc.seoul.kr
- 2Department of Radiology, First Affiliated Hospital of Nanjing Medical University, Nanjing, China.
- KMID: 1910772
- DOI: http://doi.org/10.5469/neuroint.2014.9.1.32
Abstract
- Problem with embolization of arteriovenous fistula (AVF) with liquid embolic agent is its over-penetration into the veins or regurgitation to the proximal feeder without reaching the shunt point. We present a technique that controls the flow of AVF during embolization. Two microcatheter technique consists of positioning one microcatheter close to the AVF for embolization, and with another microcatheter at the proximal feeding artery to control the AVF flow by coiling. Selective angiograms obtained using a distally positioned microcatheter before and after coiling, were compared how much stagnant effect was achieved. Using two microcatheter technique, AVF occlusion was achieved with good penetration of glue to the venous side of the AVF. Its advantage is the ability to push glue into the shunt without causing over-penetration of glue or its reflux along the feeder. Two microcatheter technique was safe and effective in glue embolization of AVF and also expected to be applied with other liquid embolic agent like Onyx.
Figure
Cited by 3 articles
-
Coil-Protected Technique for Liquid Embolization in Neurovascular Malformations
Keun Young Park, Jin Woo Kim, Byung Moon Kim, Dong Joon Kim, Joonho Chung, Chang Ki Jang, Jun-Hwee Kim
Korean J Radiol. 2019;20(8):1285-1292. doi: 10.3348/kjr.2019.0127.Embolization Tactics of Spinal Epidural Arteriovenous Fistulas
Abdulrahman Hamad Al-Abdulwahhab, Yunsun Song, Boseong Kwon, Dae Chul Suh
Neurointervention. 2021;16(3):252-259. doi: 10.5469/neuroint.2021.00220.Intrasaccular Flow Disruptor (Woven EndoBridge) Assisted Embolization of Vertebral Arteriovenous Fistulas
Oktay Algin
Neurointervention. 2024;19(1):61-64. doi: 10.5469/neuroint.2023.00514.
Reference
-
1. Kim DJ, Willinsky RA, Krings T, Agid R, Terbrugge K. Intracranial dural arteriovenous shunts: transarterial glue embolization--experience in 115 consecutive patients. Radiology. 2011; 258:554–561. PMID: 21177391.
Article2. Li MH, Tan HQ, Fang C, Zhu YQ, Wang W, Wang J, et al. Transarterial embolisation therapy of dural carotid-cavernous AVFe using low concentration n-butyl-cyanoacrylate. Acta Neurochir (Wien). 2008; 150:1149–1156. PMID: 18958391.3. Liu HM, Huang YC, Wang YH, Tu YK. Transarterial embolisation of complex cavernous sinus dural arteriovenous AVFe with low-concentration cyanoacrylate. Neuroradiology. 2000; 42:766–770. PMID: 11110083.4. Suh DC, Kim JH, Lee MS, Park S, Kim ST, Choi CG, et al. Penetration Difference of n-Butyl2-Cyanoacrylate into the Nidus in the Embolisation of Brain Arteriovenous Malformation. Interv Neuroradiol. 1998; 4:63–74. PMID: 20673392.5. Choi BS, Park JW, Kim JL, Kim SY, Park YS, Kwon HJ, et al. Treatment Strategy Based on Multimodal Management Outcome of Cavernous Sinus Dural Arteriovenous AVF (CSDAVF). Neurointervention. 2011; 6:6–12. PMID: 22125741.6. Rodesch G, Hurth M, Alvarez H, Tadie M, Lasjaunias P. Spinal cord intradural arteriovenous AVFe: anatomic, clinical, and therapeutic considerations in a series of 32 consecutive patients seen between 1981 and 2000 with emphasis on endovascular therapy. Neurosurgery. 2005; 57:973–983. PMID: 16284566.7. Jagadeesan BD, Grigoryan M, Hassan AE, Grande AW, Tummala RP. Endovascular Balloon-Assisted Embolization of Intracranial and Cervical Arteriovenous Malformations Using Dual Lumen Co-axial Balloon Microcatheters and Onyx: Initial Experience. Neurosurgery. 2013; 2. 25. [Epub ahead of print].8. Cohen JE, Moscovici S, Itshayek E. The advantages of balloon assistance in endovascular embolization of spinal dural arteriovenous AVFs. J Clin Neurosci. 2013; 20:141–143. PMID: 23146212.9. Shi ZS, Loh Y, Gonzalez N, Tateshima S, Feng L, Jahan R, et al. Flow control techniques for Onyx embolization of intracranial dural arteriovenous AVFe. J Neurointerv Surg. 2012; 5:311–316. PMID: 22591733.10. Andreou A, Ioannidis I, Nasis N. Transarterial balloon-assisted glue embolization of high-flow arteriovenous AVFs. Neuroradiology. 2008; 50:267–272. PMID: 17960371.11. Luo CB, Teng MM, Chang FC, Chang CY. Endovascular treatment of intracranial high-flow arteriovenous AVFs by Guglielmi detachable coils. J Chin Med Assoc. 2006; 69:80–85. PMID: 16570575.12. Nesbit GM, Barnwell SL. The use of electrolytically detachable coils in treating high-flow arteriovenous AVFs. AJNR Am J Neuroradiol. 1998; 19:1565–1569. PMID: 9763395.13. Lee C-S, Pyun HW, Chae EY, Kim K-K, Rhim SC, Suh DC. Reversible Aggravation of Neurological Deficits after Steroid Medication in Patients with Venous Congestive Myelopathy Caused by Spinal Arteriovenous Malformation. Interventional Neuroradiology. 2009; 15:325–329. PMID: 20465916.
Article14. Krings T, Lasjaunias PL, Hans FJ, Mull M, Nijenhuis RJ, Alvarez H, et al. Imaging in spinal vascular disease. Neuroimaging Clin N Am. 2007; 17:57–72. PMID: 17493539.
Article15. Suh DC, Kim HS, Baek HJ, Park JW, Kim KK, Rhim SC. Angioarchitecture of Spinal Dural Arteriovenous AVF - Evaluation with 3D Rotational Angiography. Neurointervention. 2012; 7:10–16. PMID: 22454779.16. Suh DC, Kim KS, Lim SM, Shi HB, Choi CG, Lee HK, et al. Technical feasibility of embolizing aneurysms with glue (N-butyl 2-cyanoacrylate): experimental study in rabbits. AJNR Am J Neuroradiol. 2003; 24:1532–1539. PMID: 13679265.17. Suh DC, Choi CG, Sung KB, Kim KK, Rhim SC. Spinal osseous epidural arteriovenous AVF with multiple small arterial feeders converging to a round AVFr nidus as a target of venous approach. AJNR Am J Neuroradiol. 2004; 25:69–73. PMID: 14729531.18. Nelson PK, Russell SM, Woo HH, Alastra AJ, Vidovich DV. Use of a wedged microcatheter for curative transarterial embolization of complex intracranial dural arteriovenous AVFs: indications, endovascular technique, and outcome in 21 patients. J Neurosurg. 2003; 98:498–506. PMID: 12650420.19. Shi HB, Suh DC, Lee HK, Lim SM, Kim DH, Choi CG, et al. Preoperative transarterial embolization of spinal tumor: embolization techniques and results. AJNR Am J Neuroradiol. 1999; 20:2009–2015. PMID: 10588136.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Snowballing Technique for High Flow Arteriovenous Fistula: A Technical Note
- Dural Arteriovenous Fistula Involving Transverse Sinus: Successful Embolization Using Onyx(R)
- Coil-Protected Technique for Liquid Embolization in Neurovascular Malformations
- Selective Arterial Embolization of Renal Arteriovenous Fistula and Arterial Aneurysm
- Iatrogenic Femoral Arteriovenous Fistulas: Endovascular Treatment with Coil Embolization in Two Patients