J Cerebrovasc Endovasc Neurosurg.
2015 Jun;17(2):85-92. 10.7461/jcen.2015.17.2.85.
Transsylvian-Transinsular Approach for Deep-Seated Basal Ganglia Hemorrhage: An Experience at a Single Institution
- Affiliations
-
- 1Department of Neurosurgery, Haeundae Paik Hospital, Inje University College of Medicine, Busan, Korea. jheaj@paik.ac.kr
- KMID: 1879339
- DOI: http://doi.org/10.7461/jcen.2015.17.2.85
Abstract
OBJECTIVE
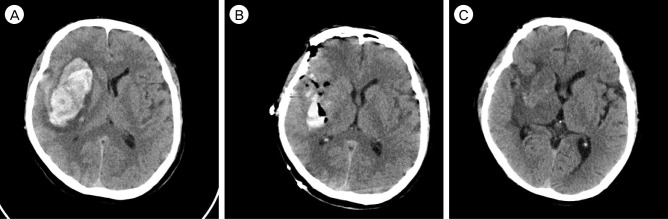
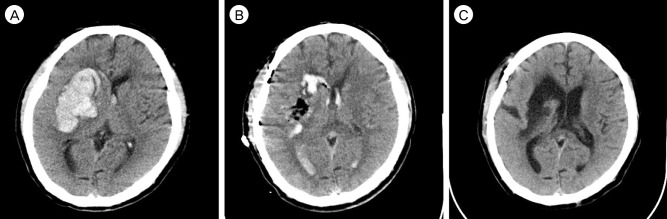
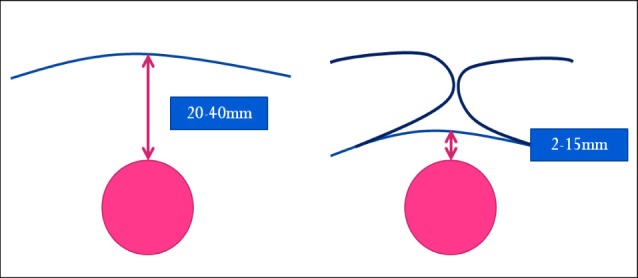
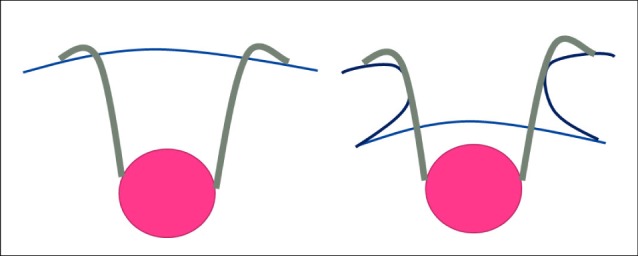
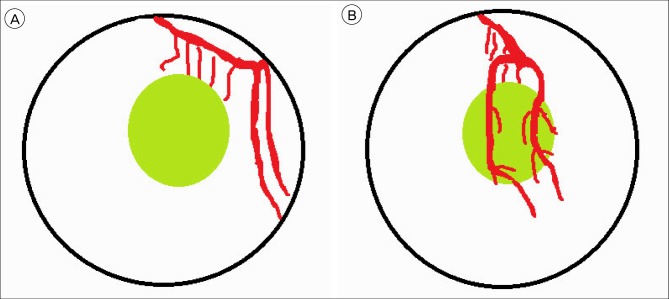
Treatment of spontaneous intracerebral hemorrhage (ICH) remains controversial. However, an extensive hemorrhage with a poor mental status is suitable for surgical evacuation. Our experience with the transsylvian-transinsular (TS-TI) microsurgical approach for deep-seated basal ganglia (BG) ICH was investigated. MATERIAL AND METHODS: A retrospective review was conducted on 86 patients with BG ICH who underwent an operation at the Department of Neurosurgery of our Hospital from September 2011 to October 2014. Thirteen patients underwent craniotomy and the TS-TI microsurgical approach for hematoma evacuation. Twenty-seven patients underwent conventional craniotomy with the trans-cortical transtemporal (TC-TT) approach, and 46 patients underwent a burrhole operation and hematoma drainage using a frameless stereotaxic device (ST).
RESULTS
The average age distribution was similar. The preoperative Glasgow coma scale (GCS) was similar for the TC-TT and TS-TI groups. The pre-operative hematoma levels were higher in the TC-TT (109.4 +/- 48.6 mL) and TS-TI (96.0 +/- 39.0 mL) groups than in the ST group (46.5 +/- 23.5 mL). The hematoma removal rate was 77% in the TC-TT group, 88% in the TS-TI group, and 34% in the ST group. The mean maintenance period of a hematoma catheter was 3.6 days in the ST group. The clinical outcome showed correlation with the preoperative neurological symptoms.
CONCLUSION
The TS-TI group was superior to the TC-TT group for evacuation of an intracerebral hematoma.
MeSH Terms
Figure
Reference
-
1. Bae HG, Lee KS, Yun IG, Bae WK, Choi SK, Byun BJ, et al. Rapid expansion of hypertensive intracerebral hemorrhage. Neurosurgery. 1992; 7. 31(1):35–41. PMID: 1641108.
Article2. Dye JA, Dusick JR, Lee DJ, Gonzalez NR, Martin NA. Frontal bur hole through an eyebrow incision for image-guided endoscopic evacuation of spontaneous intracerebral hemorrhage. J Neurosurg. 2012; 10. 117(4):767–773. PMID: 22900841.
Article3. Jianwei G, Weiqiao Z, Xiaohua Z, Qizhong L, Jiyao J, Yongming Q. Our experience of transsylvian-transinsular microsurgical approach to hypertensive putaminal hematomas. J Craniofac Surg. 2009; 7. 20(4):1097–1099. PMID: 19634217.
Article4. Kaya RA, Türkmenoğlu O, Ziyal IM, Dalkiliç T, Sahin Y, Aydin Y. The effects on prognosis of surgical treatment of hypertensive putaminal hematomas through transsylvian transinsular approach. Surg Neurol. 2003; 3. 59(3):176–183. PMID: 12681546.
Article5. Li Q, Yang CH, Xu JG, Li H, You C. Surgical treatment for large spontaneous basal ganglia hemorrhage: retrospective analysis of 253 cases. Br J Neurosurg. 2013; 10. 27(5):617–621. PMID: 23406426.
Article6. Potts MB, Chang EF, Young WL, Lawton MT. UCSF Brain AVM Study Project. Transsylvian-transinsular approaches to the insula and basal ganglia: operative techniques and results with vascular lesions. Neurosurgery. 2012; 4. 70(4):824–834. PMID: 21937930.7. Rhoton AL Jr. The supratentorial arteries. Neurosurgery. 2002; 10. 51(4 Suppl):S53–S120. PMID: 12234447.
Article8. Schaller C, Klemm E, Haun D, Schramm J, Meyer B. The transsylvian approach is "minimally invasive" but not "atraumatic". Neurosurgery. 2002; 10. 51(4):971–976. PMID: 12234405.
Article9. Schaller C, Zentner J. Vasospastic reactions in response to the transsylvian approach. Surg Neurol. 1998; 2. 49(2):170–175. PMID: 9457267.
Article10. Shin DS, Yoon SM, Kim SH, Shim JJ, Bae HG, Yun IG. Open surgical evacuation of spontaneous putaminal hematomas: prognostic factors and comparison of outcomes between transsylvian and transcortical approaches. J Korean Neurosurg Soc. 2008; 7. 44(1):1–7. PMID: 19096649.
Article11. Tanriover N, Rhoton AL Jr, Kawashima M, Ulm AJ, Yasuda A. Microsurgical anatomy of the insula and the sylvian fissure. J Neurosurg. 2004; 5. 100(5):891–922. PMID: 15137609.
Article12. Wang F, Sun T, Li X, Xia H, Li Z. Microsurgical and tractographic anatomical study of insular and transsylvian transinsular approach. Neurol Sci. 2011; 10. 32(5):865–874. PMID: 21863272.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Bilateral Traumatic Hemorrhage of the Basal Ganglia
- Traumatic Intracerebral Hemorrhage in Bilateral Basal Ganglia
- Multiple Hypertensive Intracerebral Hemorrhage: A Case Report
- Deep Cerebral Venous Thrombosis Showing Parkinsonism such as Micrographia, Hypophonia and Bradykinesia
- A Viewpoint on Treatment of Traumatic Bilateral Basal Ganglia Hemorrhage in a Child: Case Report