Tuberc Respir Dis.
2009 Mar;66(3):236-240. 10.4046/trd.2009.66.3.236.
A Case of Miliary Tuberculosis Misdiagnosed as Pneumonia and ARDS Due to the Transient Improvement after Intravenous Injection of Levofloxacin
- Affiliations
-
- 1Division of Pulmonology, Department of Internal Medicine, Konyang University College of Medicine, Daejon, Korea. sjoongkwon@hanmail.net
- 2Department of Diagnostic Radiology, Konyang University College of Medicine, Daejon, Korea.
- 3Department of Diagnostic Chest Surgery, Konyang University College of Medicine, Daejon, Korea.
- KMID: 1846387
- DOI: http://doi.org/10.4046/trd.2009.66.3.236
Abstract
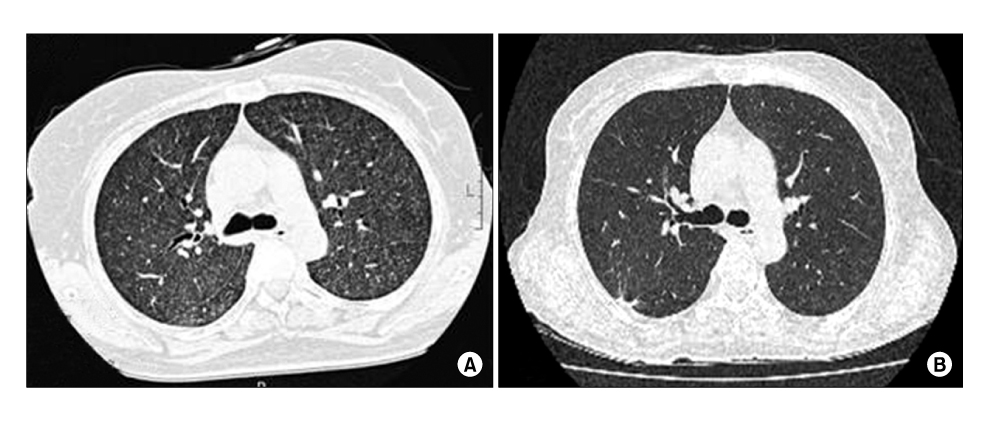
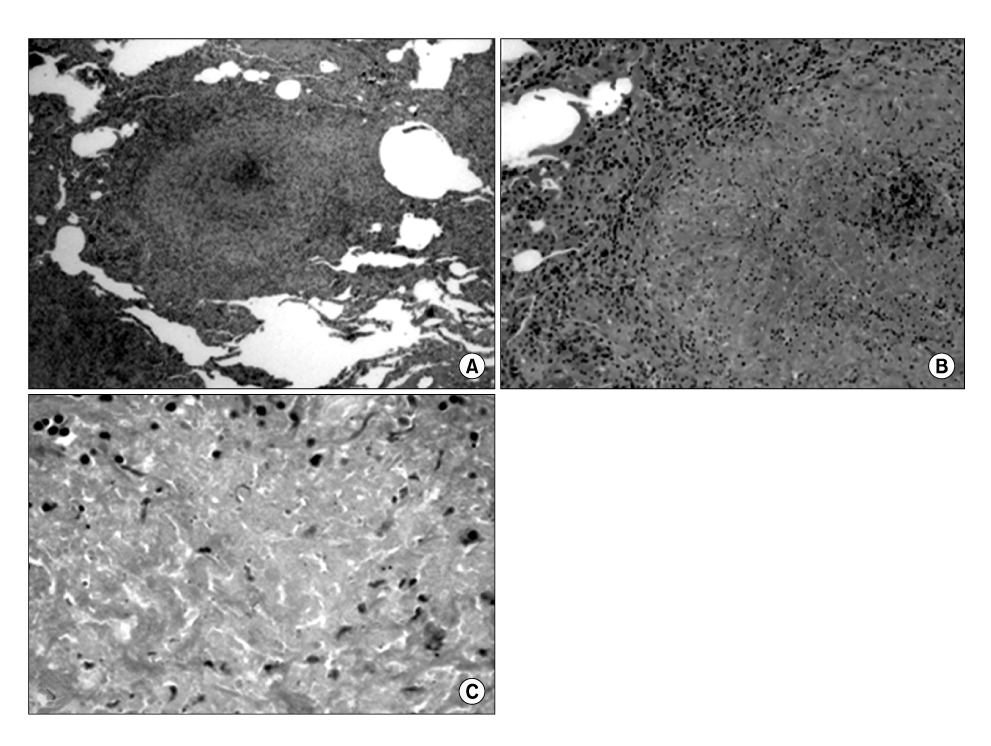
- Miliary tuberculosis is quite a rare but serious cause of acute respiratory distress syndrome (ARDS). Therefore, the early detection of military tuberculosis as the underlying cause of ARDS is very important for the prognosis and survival of the patient. We report a case of military tuberculosis mimicking ARDS. A female patient was admitted due to repeated fever and dyspnea. The initial chest CT scan showed diffuse ground glass opacity, without a miliary pattern. The case was considered to be ARDS caused by pneumonia. She showed improvement after being treated with levofloxacin. However, she was re-admitted with fever seven days after discharge. The follow up chest CT scan showed micronodules in both lungs. An open lung biopsy confirmed the diagnosis of military tuberculosis.
MeSH Terms
Figure
Reference
-
1. Rom WN, Garry SM. Baker SK, Glassroth J, editors. Miliary tuberculosis. Tuberculosis. 2004. 2th ed. Philadelphia: Lippincott Williams & Wilkins;429–432.2. Yoon YS, Lee HJ, Yoon HI, Yoo CG, Kim YW, Han SK, et al. Impact of fluoroquinolones on the diagnosis of pulmonary tuberculosis initially treated as bacterial pneumonia. Int J Tuberc Lung Dis. 2005. 9:1215–1219.3. Piqueras AR, Marruecos L, Artigas A, Rodriguez C. Miliary tuberculosis and adult respiratory distress syndrome. Intensive Care Med. 1987. 13:175–182.4. Kim JH, Jeoung CH, Kim HI, Park JH, Lee JS, Jeon GU, et al. A case report of the patient with miliary tuberculosis resulting in adult respiratory distress syndrome. Korean J Intern Med. 1986. 31:566–570.5. Bae DS, Kim JK, Kim JA, Jeon KH, Lee JH, Shine WW, et al. A clinical study of miliary tuberculosis in adults. Tuberc Respir Dis. 1984. 31:108–114.6. Ahn YS, Lee SM. A clinical review of acute respiratory distress syndrome (ARDS) due to miliary tuberculosis. Tuberc Respir Dis. 2002. 53:17–26.7. Mandell LA, Wunderink RG, Anzueto A, Bartlett JG, Campbell GD, Dean NC, et al. Infectious Diseases Society of America/American Thoracic Society consensus guidelines on the management of community-acquired pneumonia in adults. Clin Infect Dis. 2007. 44:Suppl 2. S27–S72.8. American Thoracic Society. Infectious Diseases Society of America. Guidelines for the management of adults with hospital-acquired, ventilator-associated, and healthcare-associated pneumonia. Am J Respir Crit Care Med. 2005. 171:388–416.9. Blumberg HM, Burman WJ, Chaisson RE, Daley CL, Etkind SC, Friedman LN, et al. American Thoracic Society/Centers for Disease Control and Prevention/Infectious Diseases Society of America: treatment of tuberculosis. Am J Respir Crit Care Med. 2003. 167:603–662.10. Gindburg AS, Hooper N, Parrish N, Dooley KE, Dorman SE, Booth J, et al. Fluoroquinolone resistance in patients with newly diagnosed tuberculosis. Clin Infect Dis. 2003. 37:1448–1452.11. Dooley KE, Golub J, Goes FS, Merz WG, Sterling TR. Empiric treatment of community-acquired pneumonia with fluoroquinolones, and delays in the treatment of tuberculosis. Clin Infect Dis. 2002. 34:1607–1612.12. Lee HS, Kang YA, Oh JY, Lee JH, Yoo CG, Lee CT, et al. A case of pulmonary tuberculosis with delayed diagnosis due to the temporary clinical Iimprovement after use of levofloxacin and amikacin under the impression of community acquired pneumonia. Tuberc Respir Dis. 2003. 55:395–401.13. Gaba PD, Haley C, Griffin MR, Mitchel E, Warkentin J, Holt E, et al. Increasing outpatient fluoroquinolone exposure before tuberculosis diagnosis and impact on culture-negative disease. Arch Intern Med. 2007. 167:2317–2322.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Miliary Tuberculosis Mimicking ARDS due to Bilateral Severe Pneumonia
- A Case of Pulmonary Tuberculosis with Delayed Diagnosis Due to the Temporary Clinical Improvement After Use of Levofloxacin and Amikacin Under the Impression of Community Acquired Pneumonia
- A Clinical Review of Acute Respiratory Distress Syndrome (ARDS) Due to Miliary Tuberculosis
- A Case of Acute Respiratory Distress Syndrome by Nosocomial Mycoplasma Pneumonia Associated with Cold Agglutinin Disease in Primary CNS Lymphoma
- A Case of Metastatic Tuberculosis Abscess Associated with Miliary Tuberculosis