Korean J Obstet Gynecol.
2011 Oct;54(10):634-638. 10.5468/KJOG.2011.54.10.634.
A case of squamous cell carcinoma of the uterine cervix with diffuse hematogenous lung metastasis in a 36-year-old virgin
- Affiliations
-
- 1Division of Gynecologic Oncology, Department of Obstetrics and Gynecology, Yonsei University College of Medicine, Seoul, Korea. san1@yuhs.ac
- 2Department of Obstetrics and Gynecology, The National Health Insurance Corporation Ilsan Hospital, Koyang, Korea.
- 3Department of Diagnostic Pathology, The National Health Insurance Corporation Ilsan Hospital, Koyang, Korea.
- KMID: 1836752
- DOI: http://doi.org/10.5468/KJOG.2011.54.10.634
Abstract
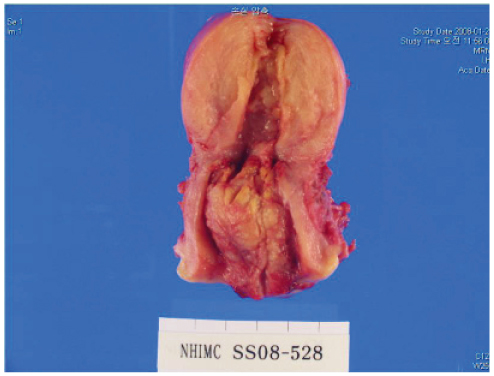
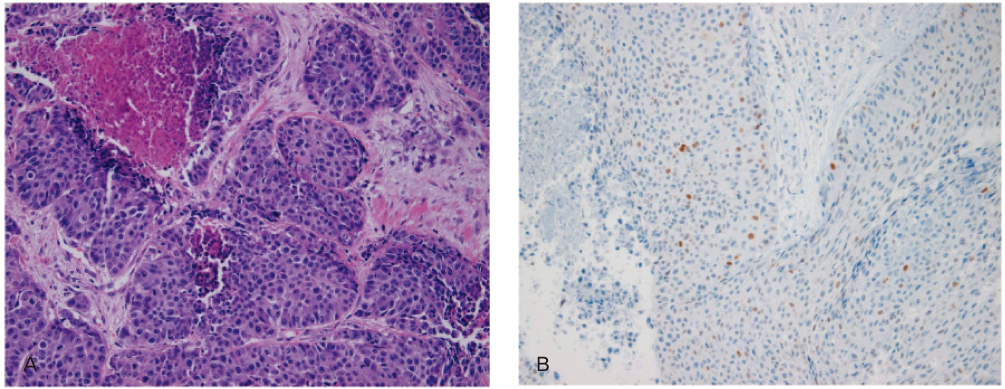
- The carcinoma of the uterine cervix in virgins is extremely rare. A 36-year-old virgin presented with a 4.8 x 2.2 cm sized endocervical mass with bleeding on sonography. Biopsy revealed a squamous cell carcinoma arising in the uterine cervix without human papilloma virus (HPV) DNA. Positron emission tomography revealed cervical cancer with multiple hematogenous lung metastases. After 3 cycles of preoperative chemotherapy, she underwent modified radical hysterectomy and 6 cycles of postoperative chemotherapy. After the treatment, complete resolution was obtained, and she has been followed without recurrence for 4 years. Although > 90% of cervical cancer is caused by HPV infection, we cannot completely deny the possibility of HPV negative cervical carcinoma.
MeSH Terms
Figure
Reference
-
1. Bosch FX, de Sanjosé S. The epidemiology of human papillomavirus infection and cervical cancer. Dis Markers. 2007. 23:213–227.2. Bosch FX, Manos MM, Muñoz N, Sherman M, Jansen AM, Peto J, et al. Prevalence of human papillomavirus in cervical cancer: a worldwide perspective. International biological study on cervical cancer (IBSCC) Study Group. J Natl Cancer Inst. 1995. 87:796–802.3. Walboomers JM, Jacobs MV, Manos MM, Bosch FX, Kummer JA, Shah KV, et al. Human papillomavirus is a necessary cause of invasive cervical cancer worldwide. J Pathol. 1999. 189:12–19.4. Wang IT, Chang CW, Tang WL, Chen WY, Liu WM. Keratinizing squamous cell carcinoma of the cervix in a sexually inexperienced woman: a case report. J Reprod Med. 2006. 51:745–746.5. Bielecki A, Borowicz K, Misiewicz L. Adenocarcinoma of the cervix uteri in a 37-year-old virgin with coexisting cancer of the body of the uterus. Am J Obstet Gynecol. 1963. 87:135–136.6. Schwarz E, Freese UK, Gissmann L, Mayer W, Roggenbuck B, Stremlau A, et al. Structure and transcription of human papillomavirus sequences in cervical carcinoma cells. Nature. 1985. 314:111–114.7. Narisawa-Saito M, Kiyono T. Basic mechanisms of high-risk human papillomavirus-induced carcinogenesis: roles of E6 and E7 proteins. Cancer Sci. 2007. 98:1505–1511.8. Wise-Draper TM, Wells SI. Papillomavirus E6 and E7 proteins and their cellular targets. Front Biosci. 2008. 13:1003–1017.9. Burger MP, Hollema H, Pieters WJ, Schröder FP, Quint WG. Epidemiological evidence of cervical intraepithelial neoplasia without the presence of human papillomavirus. Br J Cancer. 1996. 73:831–836.10. Park DJ, Wilczynski SP, Paquette RL, Miller CW, Koeffler HP. p53 mutations in HPV-negative cervical carcinoma. Oncogene. 1994. 9:205–210.11. Min-min H, Ming-rong X, Ze-yi C, Kai-xuan Y, Zhi-lin S. Analysis of p53 codon 72 polymorphism and its association with human papillomavirus 16 and 18 E6 in Chinese cervical lesions. Int J Gynecol Cancer. 2006. 16:2004–2008.12. Belhocine T, Kridelka F, Thille A, De Barsy C, Foidart-Willems J, Hustinx R, et al. Staging of primary cervical cancers: the role of nuclear medicine. Crit Rev Oncol Hematol. 2003. 46:275–284.13. Lindstrom AK, Stendahl U, Tot T, Lidström BM, Hellberg D. Predicting the outcome of squamous cell carcinoma of the uterine cervix using combinations of individual tumor marker expressions. Anticancer Res. 2007. 27:1609–1615.14. Braun K, Ehemann V, Waldeck W, Pipkorn R, Corban-Wilhelm H, Jenne J, et al. HPV18 E6 and E7 genes affect cell cycle, pRB and p53 of cervical tumor cells and represent prominent candidates for intervention by use peptide nucleic acids (PNAs). Cancer Lett. 2004. 209:37–49.15. Nair S, Pillai MR. Human papillomavirus and disease mechanisms: relevance to oral and cervical cancers. Oral Dis. 2005. 11:350–359.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Sarcomatoid squamous cell carcinoma of uterine cervix
- A Case of Duodenal Metastasis from Squamous Cell Carcinoma of the Uterine Cervix
- A Case of Metastatic Uterine Cervical Carcinma of the Orbit
- A Case of Clear Cell Adenocarcinoma in the Uterine Cervix of 22 Years-Old Virgin
- A Case of Lymphoepithelioma - Like Carcinoma of Uterine Cervix