Korean Circ J.
2011 Aug;41(8):458-463. 10.4070/kcj.2011.41.8.458.
Effect of Previous Statin Therapy in Patients With Acute Coronary Syndrome and Percutaneous Coronary Intervention
- Affiliations
-
- 1Department of Cardiovascular Medicine, Regional Cardiocerebrovascular Center, Wonkwang University Hospital, Iksan, Korea. ards7210@yahoo.co.kr
- KMID: 1826353
- DOI: http://doi.org/10.4070/kcj.2011.41.8.458
Abstract
- BACKGROUND AND OBJECTIVES
Statin therapy after percutaneous coronary intervention (PCI) has been associated with reduced major adverse cardiovascular events (MACE). However, it has been less clear as to whether statin therapy before acute coronary syndrome (ACS) is beneficial. We studied the effect of previous statin therapy, initiated > or =1 month before PCI, on the outcome of patients with ACS who had undergone early invasive strategies.
SUBJECTS AND METHODS
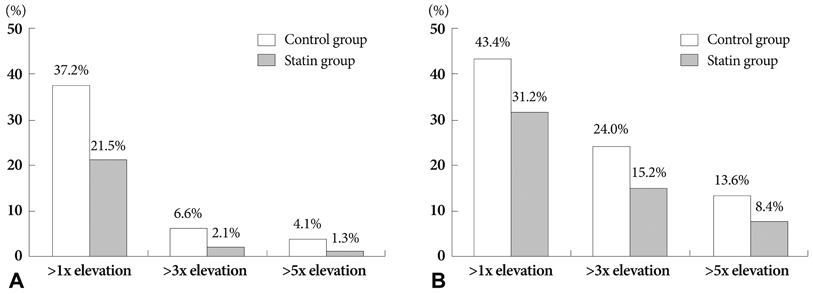
We stratified 479 consecutive patients with ACS who had undergone PCI, according to preprocedural statin administration as follows: previous statin-treated patients (statin group, n=237) and statin-naive patients (control group, n=242). The incidence of periprocedural myocardial infarction (MI) and in-hospital MACE was assessed.
RESULTS
The incidence of Braunwald class III angina and MI presentation were significantly lower in the statin group than in the control group. Angiographic and procedural characteristics were similar between the two groups; however, slow/no reflow phenomenon occurred more frequently in the control group. After PCI, the incidence of periprocedural MI was higher in the control group than in the statin group (6.6% vs. 2.1%, p=0.016). Multivariate analysis revealed that no prior use of statin {odds ratio (OR)=2.8; 95% confidence interval (CI)=1.1-7.2; p=0.038), procedural complication (OR=4.0; 95% CI=1.5-10.5; p=0.004), stent overlap (OR=4.7; 95% CI=1.3-16.4; p=0.015), and old age (OR=3.2; 95% CI=1.2-8.0; p=0.016) were independent predictors for in-hospital MACE.
CONCLUSION
Previous statin therapy before ACS was associated with milder clinical presentation and lower incidence of in-hospital MACE after early invasive strategies. The beneficial outcome is attributable to a significant reduction in periprocedural MI after PCI.
Keyword
MeSH Terms
Figure
Reference
-
1. Sacandinavian Simvastatin Survival Study (4S). Randomized trial of cholesterol lowering in 4444 patients with coronary heart disease. Lancet. 1994. 344:1383–1389.2. Shepherd J, Cobbe SM, Ford I, et al. West of Scotland Coronary Prevention Study Group. Prevention of coronary heart disease with pravastatin in men with hypercholesterolemia. N Engl J Med. 1995. 333:1301–1307.3. Sacks FM, Pfeffer MA, Moye LA, et al. Cholesterol and Recurrent Events Trial investigators. The effect of pravastatin on coronary events after myocardial infarction in patients with average cholesterol levels. N Engl J Med. 1996. 335:1001–1009.4. Long-Term Intervention with Pravastatin in Ischemic Disease (LIPID) Study Group. Prevention of cardiovascular events and death with pravastatin in patients of coronary heart disease and a board range of initial cholesterol levels. N Engl J Med. 1998. 339:1349–1357.5. Hong YJ, Jeong MH, Lim JH, et al. The prognostic significance of statin therapy according to the level of C-reactive protein in acute myocardial infarction patients who underwent percutaneous coronary intervention. Korean Circ J. 2003. 33:891–900.6. Ridker PM, Danielson E, Fonseca FA, et al. Reduction in C-reactive protein and LDL cholesterol and cardiovascular event rates after initiation of rosuvastatin: a prospective study of the JUPITER trial. Lancet. 2009. 373:1175–1182.7. Schwartz GG, Olsson AG, Ezekowitz MD, et al. Effects of atorvastatin on early recurrent ischemic events in acute coronary syndromes: the MIRACL study: a randomized controlled trial. JAMA. 2001. 285:1711–1718.8. Ray KK, Cannon CP, McCabe CH, et al. Early and late benefits of high-dose atorvastatin in patients with acute coronary syndromes: results from the PROVE IT-TIMI 22 trial. J Am Coll Cardiol. 2005. 46:1405–1410.9. Patti G, Pasceri V, Colonna G, et al. Atorvastatin pretreatment improves outcomes in patients with acute coronary syndromes undergoing early percutaneous coronary intervention: results of the ARMYDA-ACS randomized trial. J Am Coll Cardiol. 2007. 49:1272–1278.10. Yun KH, Jeong MH, Oh SK, et al. The beneficial effect of high loading dose of rosuvastatin before percutaneous coronary intervention in patients with acute coronary syndrome. Int J Cardiol. 2009. 137:246–251.11. Ishii H, Ichimiya S, Kanashiro M, et al. Effects of receipt of chronic statin therapy before the onset of acute myocardial infarction: a retrospective study in patients undergoing primary percutaneous coronary intervention. Clin Ther. 2006. 28:1812–1819.12. Chang SM, Yazbek N, Lakkis NM. Use of statins prior to percutaneous coronary intervention reduces myonecrosis and improves clinical outcome. Catheter Cardiovasc Interv. 2004. 62:193–197.13. Di Sciascio G, Patti G, Pasceri V, Gaspardone A, Colonna G, Montinaro A. Efficacy of atorvastatin reload in patients on chronic statin therapy undergoing percutaneous coronary intervention: results of the ARMYDA-RECAPTURE (Atorvastatin for Reduction of Myocardial Damage During Angioplasty) Randomized Trial. J Am Coll Cardiol. 2009. 54:558–565.14. Briguori C, Colombo A, Airoldi F, et al. Statin administration before percutaneous coronary intervention: impact on periprocedural myocardial infarction. Eur Heart J. 2004. 25:1822–1828.15. Chan AW, Bhatt DL, Chew DP, et al. Relation of inflammation and benefit of statins after percutaneous coronary interventions. Circulation. 2003. 107:1750–1756.16. Ebrahimi R, Saleh J, Toggart E, et al. Effect of preprocedural statin use on procedural myocardial infarction and major cardiac adverse events in percutaneous coronary intervention: a meta-analysis. J Invasive Cardiol. 2008. 20:292–295.17. Spencer FA, Allegrone J, Goldberg RJ, et al. Association of statin therapy with outcomes of acute coronary syndromes: the GRACE study. Ann Intern Med. 2004. 140:857–866.18. Bauer T, Bohm M, Zahn R, et al. Effect of chronic statin pretreatment on hospital outcome in patients with acute non-ST-elevation myocardial infarction. J Cardiovasc Pharmacol. 2009. 53:132–136.19. Takemoto M, Liao JK. Pleiotropic effects of 3-hydroxy-3-methylglutaryl coenzyme a reductase inhibitors. Arterioscler Thromb Vasc Biol. 2001. 21:1712–1719.20. Sposito AC, Chapman MJ. Statin therapy in acute coronary syndromes: mechanistic insight into clinical benefit. Arterioscler Thromb Vasc Biol. 2002. 22:1524–1534.21. Rhee SJ, Yun KH, Oh SK, et al. Changes of C-reactive protein are associated with myocardial injury after successful percutaneous coronary intervention. Korean Circ J. 2008. 38:135–139.22. Choi SY, Yang HM, Tahk SJ, et al. Preprocedural hs-CRP level serves as a marker for procedure-related myocardial injury during coronary stenting. Korean Circ J. 2005. 35:140–148.23. Yun KH, Jeong MH, Oh SK, et al. Response of high-sensitivity C-reactive protein to percutaneous coronary intervention in patients with acute coronary syndrome. Heart Vessels. 2009. 24:175–180.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Staged versus One-Time Percutaneous Coronary Intervention Strategy for Multivessel Non-ST Segment Elevation Acute Coronary Syndrome
- Recent Advances in Percutaneous Coronary Intervention in Coronary Artery Disease
- Statin Therapy with Coronary Plaque Imaging
- Antiplate Agents
- De-escalation strategies of dual antiplatelet therapy in patients undergoing percutaneous coronary intervention for acute coronary syndrome