J Korean Soc Transplant.
2009 Dec;23(3):214-226. 10.4285/jkstn.2009.23.3.214.
Current Strategies for Successful Islet Xenotransplantation
- Affiliations
-
- 1Transplantation Research Institute, Seoul National University Medical Research Center, Seoul, Korea.
- 2Transplantation Center Seoul National University Hospital, Transplantation Research Institute, Seoul National University Medical Research Center, Seoul, Korea.
- 3Division of Nephrology, Transplantation Research Institute, Seoul National University Medical Research Center, Seoul, Korea. curie@snu.ac.kr
- KMID: 1819843
- DOI: http://doi.org/10.4285/jkstn.2009.23.3.214
Abstract
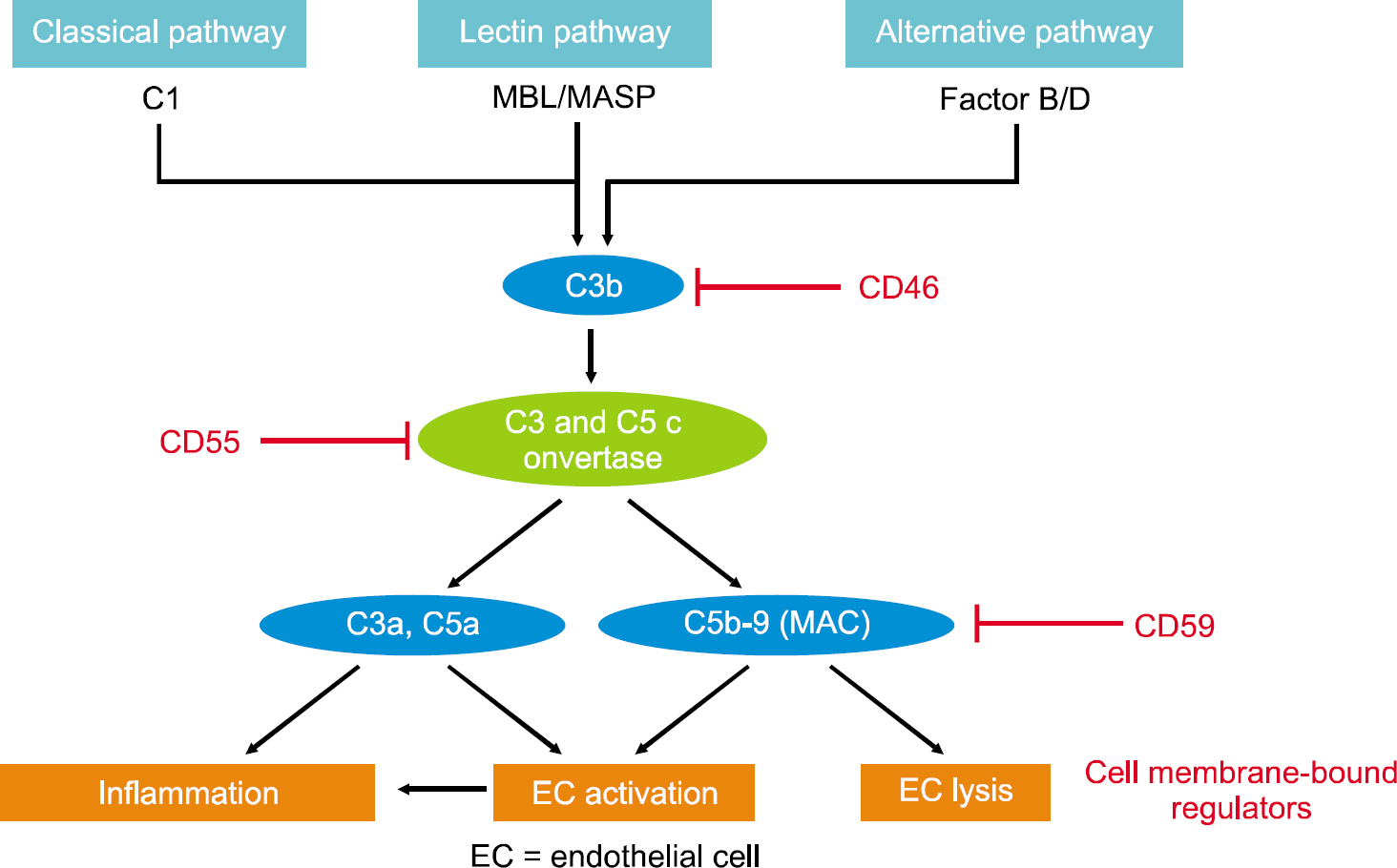
- Diabetes mellitus is increasing all over the world and is a serious health problem. Pancreatic islet transplantation is promising treatment for diabetes mellitus, but an imbalance between deceased pancreas donors and recipients limited the widespread clinical application. Therefore, pig islets could be used as an alternative islet source in transplantation. However, a big hurdle to clinical application of islet xenotransplantation is the instant blood mediated inflammatory reaction (IBMIR), which is characterized by activation of the coagulation cascade, platelets and complement systems. Innate immune cells infiltrate the islets in the process of IBMIR and thereby accelerate the early graft loss. Characteristics of IBMIR in islet xenotransplantion are very different from the rejection in solid organ xenotransplantation. Therefore, we focus on the molecules for surmounting IBMIR in order to accomplish successful islet xenotransplantation. To prevent the IBMIR in islet xenotransplantation, development of genetic modified pigs containing anti-coagulant, anti-thrombosis and complement regulatory genes, or capsulation of islet with biomaterials for blocking immune response around islet surface can be tried. Galpha-Gal knockout pigs and the diverse transgenic pigs for complement regulatory protein or anti-coagulant genes have been developed for xenotransplantation. This review summarized on characteristics of rejection in islet xenotransplantation and discusses the strategies for overcoming the rejection.
Keyword
MeSH Terms
Figure
Reference
-
1). Zimmet P, Alberti KG, Shaw J. Global and societal implications of the diabetes epidemic. Nature. 2001; 414:782–7.
Article2). Korea National Health and Nutrition Examination Survey. Korea National Health and Nutrition Examination Survey 2005 [Internet]. Seoul: The Korea Centers for Disease Control and Prevention;2009. Available from. http://knhanes.cdc.go.kr.3). Scharp DW, Lacy PE, Santiago JV, McCullough CS, Weide LG, Falqui L, et al. Insulin independence after islet transplantation into type I diabetic patient. Diabetes. 1990; 39:515–8.
Article4). Park JB, Kim SJ. Clinical islet transplantation: where do we stand on? J Korean Soc Transplant. 2007; 21:196–202.5). Shapiro AM, Lakey JR, Ryan EA, Korbutt GS, Toth E, Warnock GL, et al. Islet transplantation in seven patients with type 1 diabetes mellitus using a glucocorticoid-free immunosuppressive regimen. N Engl J Med. 2000; 343:230–8.
Article6). Rood PP, Buhler LH, Bottino R, Trucco M, Cooper DK. Pig-to-nonhuman primate islet xenotransplantation: a review of current problems. Cell Transplant. 2006; 15:89–104.
Article7). Reemtsma K, McCracken BH, Schlegel JU, Pearl MA, Pearce CW, Dewitt CW, et al. Renal heterotransplantation in man. Ann Surg. 1964; 160:384–410.
Article8). Bailey LL, Nehlsen-Cannarella SL, Concepcion W, Jolley WB. Baboon-to-human cardiac xenotransplantation in a neonate. JAMA. 1985; 254:3321–9.
Article9). Pruitt SK, Kirk AD, Bollinger RR, Marsh HC Jr, Collins BH, Levin JL, et al. The effect of soluble complement receptor type 1 on hyperacute rejection of porcine xenografts. Transplantation. 1994; 57:363–70.
Article10). Tseng YL, Kuwaki K, Dor FJ, Shimizu A, Houser S, Hisashi Y, et al. alpha1,3-Galactosyltransferase gene-knockout pig heart transplantation in baboons with survival approaching 6 months. Transplantation. 2005; 80:1493–500.11). Rayat GR, Gill RG. Indefinite survival of neonatal porcine islet xenografts by simultaneous targeting of LFA-1 and CD154 or CD45RB. Diabetes. 2005; 54:443–51.
Article12). Choi I, Kim SD, Cho B, Kim D, Park D, Koh HS, et al. Xenogeneic interaction between human CD40L and porcine CD40 activates porcine endothelial cells through NF-kappaB signaling. Mol Immunol. 2008; 45:575–80.13). Ahn C, et al. Fgl2 induction in porcine endothelial cells through xenogeneic CD40-CD40L interaction. (in press).14). Lee EM, Park JO, Kim D, Kim JY, Oh KH, Park CG, et al. Early up-regulation of CXC-chemokine expression is associated with strong cellular immune responses to murine skin xenografts. Xenotransplantation. 2006; 13:328–36.
Article15). Kim JY, Kim D, Lee EM, Choi I, Park CG, Kim KS, et al. Inducible nitric oxide synthase inhibitors prolonged the survival of skin xenografts through selective down- regulation of pro-inflammatory cytokine and CC-chemo-kine expressions. Transpl Immunol. 2003; 12:63–72.16). Yang J, Cho B, Choi I, Kim DH, Kim SD, Koh HS, et al. Molecular characterization of miniature porcine RANTES and its chemotactic effect on human mononuclear cells. Transplantation. 2006; 82:1229–33.
Article17). Yang J, Choi I, Kim SD, Kim ES, Cho B, Kim JY, et al. Molecular characterization of cDNA encoding porcine IP-10 and induction of porcine endothelial IP-10 in response to human TNF-alpha. Vet Immunol Immunopathol. 2007; 117:124–8.18). Choi I, Cho B, Kim SD, Park D, Kim JY, Park CG, et al. Molecular cloning, expression and functional characterization of miniature swine CD86. Mol Immunol. 2006; 43:480–6.
Article19). Nilsson B. The instant blood-mediated inflammatory reaction in xenogeneic islet transplantation. Xenotransplantation. 2008; 15:96–8.
Article20). Bennet W, Groth CG, Larsson R, Nilsson B, Korsgren O. Isolated human islets trigger an instant blood mediated inflammatory reaction: implications for intraportal islet transplantation as a treatment for patients with type 1 diabetes. Ups J Med Sci. 2000; 105:125–33.
Article21). Bennet W, Sundberg B, Groth CG, Brendel MD, Brandhorst D, Brandhorst H, et al. Incompatibility between human blood and isolated islets of Langerhans: a finding with implications for clinical intraportal islet transplantation? Diabetes. 1999; 48:1907–14.
Article22). Bühler L, Deng S, O'Neil J, Kitamura H, Koulmanda M, Baldi A, et al. Adult porcine islet transplantation in baboons treated with conventional immunosuppression or a non-myeloablative regimen and CD154 blockade. Xenotransplantation. 2002; 9:3–13.
Article23). van der Windt DJ, Bottino R, Casu A, Campanile N, Cooper DK. Rapid loss of intraportally transplanted islets: an overview of pathophysiology and preventive strategies. Xenotransplantation. 2007; 14:288–97.
Article24). Cowan PJ. Coagulation and the xenograft endothelium. Xenotransplantation. 2007; 14:7–12.
Article25). Lin CC, Chen D, McVey JH, Cooper DK, Dorling A. Expression of tissue factor and initiation of clotting by human platelets and monocytes after incubation with porcine endothelial cells. Transplantation. 2008; 86:702–9.
Article26). Glaser CB, Morser J, Clarke JH, Blasko E, McLean K, Kuhn I, et al. Oxidation of a specific methionine in thrombomodulin by activated neutrophil products blocks cofactor activity. A potential rapid mechanism for modu-lation of coagulation. J Clin Invest. 1992; 90:2565–73.
Article27). Stearns-Kurosawa DJ, Kurosawa S, Mollica JS, Ferrell GL, Esmon CT. The endothelial cell protein C receptor augments protein C activation by the thrombin-throm-bomodulin complex. Proc Natl Acad Sci USA. 1996; 93.
Article28). Taylor FB Jr, Peer GT, Lockhart MS, Ferrell G, Esmon CT. Endothelial cell protein C receptor plays an im-portant role in protein C activation in vivo. Blood. 2001; 97:1685–8.29). Pike RN, Buckle AM, Le Bonniec BF, Church FC. Control of the coagulation system by serpins. Getting by with a little help from glycosaminoglycans. FEBS J. 2005; 272:4842–51.30). Dwyer KM, Mysore TB, Crikis S, Robson SC, Nandurkar H, Cowan PJ, et al. The transgenic expression of human CD39 on murine islets inhibits clotting of human blood. Transplantation. 2006; 82:428–32.
Article31). Dwyer KM, Deaglio S, Gao W, Friedman D, Strom TB, Robson SC. CD39 and control of cellular immune responses. Purinergic Signal. 2007; 3:171–80.
Article32). Shimizu A, Hisashi Y, Kuwaki K, Tseng YL, Dor FJ, Houser SL, et al. Thrombotic microangiopathy associated with humoral rejection of cardiac xenografts from alpha1,3-galacto-syltransferase gene-knockout pigs in baboons. Am J Pathol. 2008; 172:1471–81.33). Cooper DK, Good AH, Koren E, Oriol R, Malcolm AJ, Ippolito RM, et al. Identification of alpha-galactosyl and other carbohydrate epitopes that are bound by human an-ti-pig antibodies: relevance to discordant xenografting in man. Transpl Immunol. 1993; 1:198–205.34). Rood PP, Bottino R, Balamurugan AN, Smetanka C, Ayares D, Groth CG, et al. Reduction of early graft loss after intraportal porcine islet transplantation in monkeys. Transplantation. 2007; 83:202–10.
Article35). Rayat GR, Rajotte RV, Hering BJ, Binette TM, Korbutt GS. In vitro and in vivo expression of Galalpha-(1,3)Gal on porcine islet cells is age dependent. J Endocrinol. 2003; 177:127–35.36). Hering BJ, Kandaswamy R, Harmon JV, Ansite JD, Clemmings SM, Sakai T, et al. Transplantation of cul-tured islets from two-layer preserved pancreases in type 1 diabetes with anti-CD3 antibody. Am J Transplant. 2004; 4:390–401.
Article37). Mohanakumar T, Narayanan K, Desai N, Ramachandran S, Shenoy S, Jendrisak M, et al. A significant role for histocompatibility in human islet transplantation. Transplantation. 2006; 82:180–7.
Article38). Huber-Lang M, Sarma JV, Zetoune FS, Rittirsch D, Neff TA, McGuire SR, et al. Generation of C5a in the absence of C3: a new complement activation pathway. Nat Med. 2006; 12:682–7.
Article39). Janeway CA Jr, Travers P, Walport M, Shlomchik MJ. Immunobiology: the immune system in health and disease. 6th ed.New York: Garland Science;2005. p. 55–75.40). Kues WA, Schwinzer R, Wirth D, Verhoeyen E, Lemme E, Herrmann D, et al. Epigenetic silencing and tissue in-dependent expression of a novel tetracycline inducible system in double-transgenic pigs. FASEB J. 2006; 20:1200–2.
Article41). Cowan PJ, Aminian A, Barlow H, Brown AA, Chen CG, Fisicaro N, et al. Renal xenografts from triple-transgenic pigs are not hyperacutely rejected but cause coagulopathy in non-immunosuppressed baboons. Transplantation. 2000; 27:69. 2504–15.
Article42). Bennet W, Björkland A, Sundberg B, Brandhorst D, Brendel MD, Richards A, et al. Expression of complement regulatory proteins on islets of Langerhans: a com-parison between human islets and islets isolated from normal and hDAF transgenic pigs. Transplantation. 2001; 72:312–9.43). van der Windt DJ, Bottino R, Casu A, Campanile N, Smetanka C, He J, et al. Long-term controlled normogly-cemia in diabetic non-human primates after transplantation with hCD46 transgenic porcine islets. Am J Transplant. 2009; 9:2716–26.
Article44). Shrivastava S, McVey JH, Dorling A. The interface between coagulation and immunity. Am J Transplant. 2007; 7:499–506.
Article45). Contreras JL, Eckstein C, Smyth CA, Bilbao G, Vilatoba M, Ringland SE, et al. Activated protein C preserves functional islet mass after intraportal transplantation: a novel link between endothelial cell activation, thrombosis, inflammation, and islet cell death. Diabetes. 2004; 53:2804–14.46). Coughlin SR. Thrombin signalling and protease-activated receptors. Nature. 2000; 407:258–64.
Article47). Moberg L, Korsgren O, Nilsson B. Neutrophilic gran-ulocytes are the predominant cell type infiltrating pancreatic islets in contact with ABO-compatible blood. Clin Exp Immunol. 2005; 142:125–31.
Article48). Ozmen L, Ekdahl KN, Elgue G, Larsson R, Korsgren O, Nilsson B. Inhibition of thrombin abrogates the instant blood-mediated inflammatory reaction triggered by isolated human islets: possible application of the thrombin inhibitor melagatran in clinical islet transplantation. Diabetes. 2002; 51:1779–84.49). Bottino R, Balamurugan AN, Tse H, Thirunavukkarasu C, Ge X, Profozich J, et al. Response of human islets to isolation stress and the effect of antioxidant treatment. Diabetes. 2004; 53:2559–68.
Article50). Hanley S, Liu S, Lipsett M, Castellarin M, Rosenberg L, Tchervenkov J, et al. Tumor necrosis factor alpha production by human islets leads to postisolation cell death. Transplantation. 2006; 82:813–18.51). Langford GA, Yannoutsos N, Cozzi E, Lancaster R, Elsome K, Chen P, et al. Production of pigs transgenic for human decay accelerating factor. Transplant Proc. 1994; 26:1400–1.52). Murakami H, Nagashima H, Takahagi Y, Miyagawa S, Fujimura T, Toyomura K, et al. Transgenic pigs expressing human decay-accelerating factor regulated by porcine MCP gene promoter. Mol Reprod Dev. 2002; 61:302–11.
Article53). Zhou CY, McInnes E, Copeman L, Langford G, Parsons N, Lancaster R, et al. Transgenic pigs expressing human CD59, in combination with human membrane cofactor protein and human decay-accelerating factor. Xenotransplantation. 2005; 12:142–8.
Article54). Lai L, Kolber-Simonds D, Park KW, Cheong HT, Greenstein JL, Im GS, et al. Production of alpha-1,3-gal-actosyltransferase knockout pigs by nuclear transfer cloning. Science. 2002; 295:1089–92.55). Phelps CJ, Koike C, Vaught TD, Boone J, Wells KD, Chen SH, et al. Production of alpha 1,3-galactosyl-transferase-deficient pigs. Science. 2003; 299:411–4.56). Tu CF, Hsieh SL, Lee JM, Yang LL, Sato T, Lee KH, et al. Successful generation of transgenic pigs for human decay-accelerating factor and human leucocyte antigen DQ. Transplant Proc. 2000; 32:913–5.
Article57). Ramsoondar JJ, Macháty Z, Costa C, Williams BL, Fodor WL, Bondioli KR. Production of alpha 1,3-galactosyl-transferase-knockout cloned pigs expressing human alpha 1,2-fucosylosyltransferase. Biol Reprod. 2003; 69:437–45.58). Lee S, Chung J, Ha IS, Yi K, Lee JE, Kang HG, et al. Hydrogen peroxide increases human leukocyte adhesion to porcine aortic endothelial cells via NFkappaB-depend-ent up-regulation of VCAM-1. Int Immunol. 2007; 19:1349–59.59). Hancock WW, Buelow R, Sayegh MH, Turka LA. Antibody-induced transplant arteriosclerosis is prevented by graft expression of antioxidant and anti-apoptotic genes. Nat Med. 1998; 4:1392–6.
Article60). de Vos P, Faas MM, Strand B, Calafiore R. Alginate- based microcapsules for immunoisolation of pancreatic islets. Biomaterials. 2006; 27:5603–17.61). Stabler CL, Sun XL, Cui W, Wilson JT, Haller CA, Chaikof EL. Surface re-engineering of pancreatic islets with re-combinant azido-thrombomodulin. Bioconjug Chem. 2007; 18:1713–5.
Article62). Kin T, O'Neil JJ, Pawlick R, Korbutt GS, Shapiro AM, Lakey JR. The use of an approved biodegradable polymer scaffold as a solid support system for improvement of islet engraftment. Artif Organs. 2008; 32:990–3.
Article63). Berman DM, O'Neil JJ, Coffey LC, Chaffanjon PC, Kenyon NM, Ruiz P Jr, et al. Long-term survival of non-human primate islets implanted in an omental pouch on a biodegradable scaffold. Am J Transplant. 2009; 9:91–104.
Article64). Dufour JM, Rajotte RV, Zimmerman M, Rezania A, Kin T, Dixon DE, et al. Development of an ectopic site for islet transplantation, using biodegradable scaffolds. Tissue Eng. 2005; 11:1323–31.
Article65). Hering BJ, Wijkstrom M, Graham ML, Hårdstedt M, Aasheim TC, Jie T, et al. Prolonged diabetes reversal after intraportal xenotransplantation of wild-type porcine islets in immunosuppressed nonhuman primates. Nat Med. 2006; 12:301–3.
Article66). Cardona K, Korbutt GS, Milas Z, Lyon J, Cano J, Jiang W, et al. Long-term survival of neonatal porcine islets in nonhuman primates by targeting costimulation pathways. Nat Med. 2006; 12:304–6.
Article67). Dufrane D, Goebbels RM, Saliez A, Guiot Y, Gianello P. Six-month survival of microencapsulated pig islets and alginate biocompatibility in primates: proof of concept. Transplantation. 2006; 81:1345–53.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- History, current status and perspective of islet transplantation
- Current Status and Future Perspectives of Xenotransplantation
- Current Status of Solid Organ Xenotransplantation
- Pancreas and Islet Transplantation in Diabetes
- Implications of Calcineurin/NFAT Inhibitors' Regulation of Dendritic Cells and Innate Immune Cells in Islet Xenotransplantation