J Korean Fract Soc.
2014 Jan;27(1):17-22. 10.12671/jkfs.2014.27.1.17.
Neurologic Injury within Pelvic Ring Injuries
- Affiliations
-
- 1Department of Orthopedic Surgery, Haeundae Paik Hospital, Inje University College of Medicine, Busan, Korea. cocopam76@naver.com
- KMID: 1816997
- DOI: http://doi.org/10.12671/jkfs.2014.27.1.17
Abstract
- PURPOSE
To evaluate the incidence of neurologic injury in pelvic ring injuries and to assess the risk factors for neurologic injury related to pelvic fractures.
MATERIALS AND METHODS
Sixty-two patients with the pelvic ring injury were enrolled in the study from March 2010 to May 2013. When the neurologic injury was suspected clinically, the electro-diagnostic tests were performed. Combined injuries, fracture types, and longitudinal displacements were examined for correlations with the neurologic injury.
RESULTS
There were 7 cases of AO/OTA type A, 37 cases of type B, and 18 cases of type C. Among them, 25 patients (40%) had combined spine fractures, and the average of longitudinal displacement was 7 mm (1-50 mm). Of the 62 patients, 13 (21%) had neurologic injury related with pelvic fractures; 5 with lumbosacral plexus injury, 5 with L5 or S1 nerve injury, 2 with obturator nerve injury, and 1 case of lateral femoral cutaneous nerve injury. There were no relationships between the neurologic injuries and fracture types (p=0.192), but the longitudinal displacements of posterior ring and combined spine fractures were related to the neurologic injury within pelvic ring injury (p=0.006, p=0.048).
CONCLUSION
The incidence of neurologic injury in pelvis fracture was 21%. In this study, the longitudinal displacements of posterior ring and combined spine fractures were risk factors for neurological injury in pelvic ring injury.
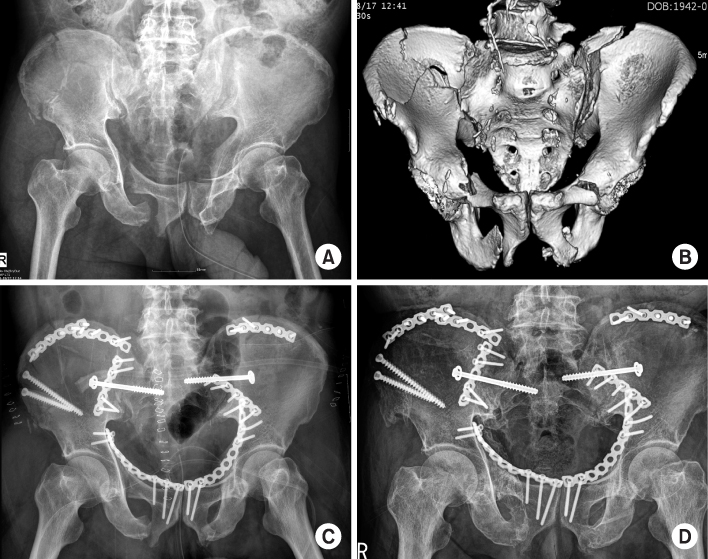
Figure
Cited by 1 articles
-
Surgical Outcome of Posterior Pelvic Fixation Using S1, S2 Screws in Vertically Unstable Pelvic Ring Injury
Kwang Hee Yeo, Nam Hoon Moon, Jae Min Ahn, Jae Yoon Jeong, Jae Hoon Jang
J Korean Fract Soc. 2018;31(1):9-17. doi: 10.12671/jkfs.2018.31.1.9.
Reference
-
1. Atlihan D, Tekdemir I, Ateŝ Y, Elhan A. Anatomy of the anterior sacroiliac joint with reference tolumbosacral nerves. Clin Orthop Relat Res. 2000; (376):236–241.2. Balogh Z, Caldwell E, Heetveld M, et al. Institutional practice guidelines on management of pelvic fracture-related hemodynamic instability: do they make a difference? J Trauma. 2005; 58:778–782.
Article3. Chin CH, Chew KC. Lumbosacral nerve root avulsion. Injury. 1997; 28:674–678.
Article4. Chiou-Tan FY, Kemp K Jr, Elfenbaum M, Chan KT, Song J. Lumbosacral plexopathy in gunshot wounds and motor vehicle accidents: comparison of electrophysiologic findings. Am J Phys Med Rehabil. 2001; 80:280–285.5. Denis F, Davis S, Comfort T. Sacral fractures: an important problem. Retrospective analysis of 236 cases. Clin Orthop Relat Res. 1988; 227:67–81.6. Ebraheim NA, Lu J, Biyani A, Huntoon M, Yeasting RA. The relationship of lumbosacral plexus to the sacrum and the sacroiliac joint. Am J Orthop (Belle Mead NJ). 1997; 26:105–110.7. Gänsslen A, Pohlemann T, Paul C, Lobenhoffer P, Tscherne H. Epidemiology of pelvic ring injuries. Injury. 1996; 27:Suppl 1. S-A13-20.
Article8. Huittinen VM. Lumbosacral nerve injury in fracture of the pelvis. A postmortem radiographic and patho-anatomical study. Acta Chir Scand Suppl. 1972; 429:3–43.9. Kim JW, Hong SK, Kyoung KH, Choi JH, Kim JJ. Comparison of the mortality rate according to the presence of trauma team in hemodynamically unstable patients with pelvic ring injury. J Korean Orthop Assoc. 2012; 47:191–197.
Article10. Kutsy RL, Robinson LR, Routt ML Jr. Lumbosacral plexopathy in pelvic trauma. Muscle Nerve. 2000; 23:1757–1760.
Article11. Lam CR. Nerve injury in fracture of the pelvis. Ann Surg. 1936; 104:945–951.
Article12. Lang EM, Borges J, Carlstedt T. Surgical treatment of lumbosacral plexus injuries. J Neurosurg Spine. 2004; 1:64–71.
Article13. Majeed SA. Neurologic deficits in major pelvic injuries. Clin Orthop Relat Res. 1992; (282):222–228.
Article14. McMurtry R, Walton D, Dickinson D, Kellam J, Tile M. Pelvic disruption in the polytraumatized patient: a management protocol. Clin Orthop Relat Res. 1980; (151):22–30.15. Patterson FP, Morton KS. Neurological complications of fractures and dislocations of the pelvis. J Trauma. 1972; 12:1013–1023.
Article16. Rai SK, Far RF, Ghovanlou B. Neurologic deficits associated with sacral wing fractures. Orthopedics. 1990; 13:1363–1366.
Article17. Reilly MC, Zinar DM, Matta JM. Neurologic injuries in pelvic ring fractures. Clin Orthop Relat Res. 1996; (329):28–36.
Article18. Schmal H, Hauschild O, Culemann U, et al. Identification of risk factors for neurological deficits in patients with pelvic fractures. Orthopedics. 2010; 33.
Article19. Smith W, Williams A, Agudelo J, et al. Early predictors of mortality in hemodynamically unstable pelvis fractures. J Orthop Trauma. 2007; 21:31–37.
Article20. Sugimoto Y, Ito Y, Tomioka M, et al. Risk factors for lumbosacral plexus palsy related to pelvic fracture. Spine (Phila Pa 1976). 2010; 35:963–966.
Article21. Tonetti J, Cazal C, Eid A, et al. Neurological damage in pelvic injuries: a continuous prospective series of 50 pelvic injuries treated with an iliosacral lag screw. Rev Chir Orthop Reparatrice Appar Mot. 2004; 90:122–131.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Delayed bladder perforation due to screw loosening after pelvic ring injury surgery: a case report
- Testicular Dislocation Associated with Pelvic Ring Injury
- External iliac artery injury with posterior pelvic ring injury in Korea: a report of two cases
- Treatment of Unstable Pelvic Ring Injuries
- Operative Treatment of Unstable Pelvic Ring Injury