J Gynecol Oncol.
2014 Jan;25(1):64-69. 10.3802/jgo.2014.25.1.64.
Surgical anatomy of the common iliac veins during para-aortic and pelvic lymphadenectomy for gynecologic cancer
- Affiliations
-
- 1Department of Gynecology, Chiba University School of Medicine, Chiba, Japan. kazuyoshi.kato@jfcr.or.jp
- KMID: 1811190
- DOI: http://doi.org/10.3802/jgo.2014.25.1.64
Abstract
OBJECTIVE
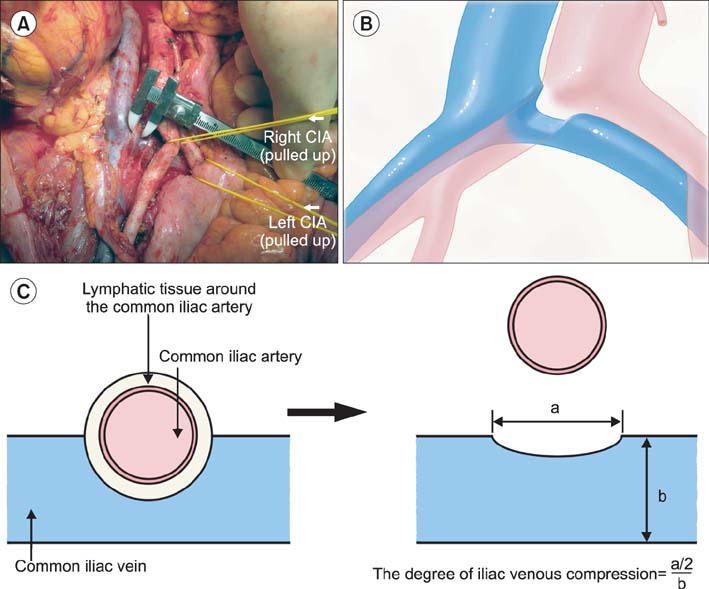
Compression of the left common iliac vein between the right common iliac artery and the vertebrae is known to be associated with the occurrence of left iliofemoral deep vein thrombosis (DVT). In this study, we described the variability in vascular anatomy of the common iliac veins and evaluated the relationship between the degree of iliac vein compression and the presence of DVT using the data from surgeries for gynecologic cancer.
METHODS
The anatomical variations and the degrees of iliac vein compression were determined in 119 patients who underwent systematic para-aortic and pelvic lymphadenectomy during surgery for primary gynecologic cancer. Their medical records were reviewed with respect to patient-, disease-, and surgery-related data.
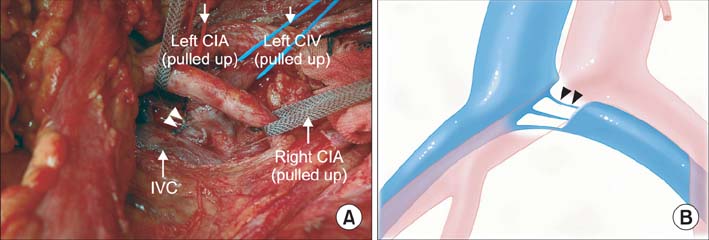
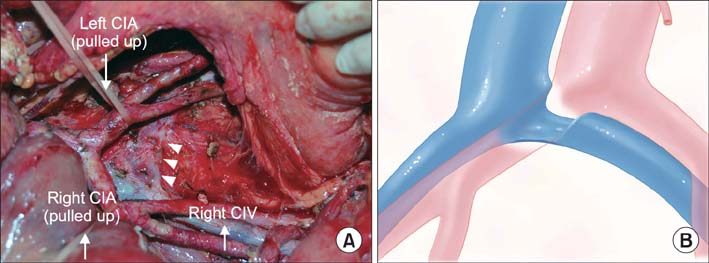
RESULTS
The degrees of common iliac vein compression were classified into three grades: grade A (n=28, 23.5%), with a calculated percentage of 0%-25% compression; grade B (n=47, 39.5%), with a calculated percentage of 26%-50% compression; and grade C (n=44, 37%), with a calculated percentage of more than 50% compression. Seven patients (5.9%) had common iliac veins with anomalous anatomies; three were divided into small caliber vessels, two with a flattened structure, and two had double inferior vena cavae. The presence of DVT was associated with the elevated D-dimer levels but not with the degree of iliac vein compression in this series.
CONCLUSION
Although severe compression of the common iliac veins was frequently observed, the degree of compression might not be associated with DVT in surgical patients with gynecologic cancer. Anomalous anatomies of common iliac veins should be considered during systematic para-aortic and pelvic lymphadenectomy in the gynecologic cancer patients.
MeSH Terms
Figure
Reference
-
1. Chang SJ, Bristow RE, Ryu HS. Analysis of para-aortic lymphadenectomy up to the level of the renal vessels in apparent earlystage ovarian cancer. J Gynecol Oncol. 2013; 24:29–36.2. Kim HS, Ju W, Jee BC, Kim YB, Park NH, Song YS, et al. Systematic lymphadenectomy for survival in epithelial ovarian cancer: a meta-analysis. Int J Gynecol Cancer. 2010; 20:520–528.3. ASTEC study group. Kitchener H, Swart AM, Qian Q, Amos C, Parmar MK. Efficacy of systematic pelvic lymphadenectomy in endometrial cancer (MRC ASTEC trial): a randomised study. Lancet. 2009; 373:125–136.4. Benedetti Panici P, Basile S, Maneschi F, Alberto Lissoni A, Signorelli M, Scambia G, et al. Systematic pelvic lymphadenectomy vs. no lymphadenectomy in early-stage endometrial carcinoma: randomized clinical trial. J Natl Cancer Inst. 2008; 100:1707–1716.5. Todo Y, Kato H, Kaneuchi M, Watari H, Takeda M, Sakuragi N. Survival effect of para-aortic lymphadenectomy in endometrial cancer (SEPAL study): a retrospective cohort analysis. Lancet. 2010; 375:1165–1172.6. Wright JD, Herzog TJ, Abu-Rustum NR. Cytoreductive surgery: abdominal retroperitoneum and adenopathy. In : Bristow RE, Karlan BY, Chi DS, editors. Surgery for ovarian cancer. 2nd ed. New York: Informa Healthcare;2010. p. 122–139.7. May R, Thurner J. The cause of the predominately sinistral occurrence of thrombosis of the pelvic veins. Angiology. 1957; 8:419–427.8. Cockett FB, Thomas ML. The iliac compression syndrome. Br J Surg. 1965; 52:816–821.9. Kibbe MR, Ujiki M, Goodwin AL, Eskandari M, Yao J, Matsumura J. Iliac vein compression in an asymptomatic patient population. J Vasc Surg. 2004; 39:937–943.10. Satoh T, Matsumoto K, Uno K, Sakurai M, Okada S, Onuki M, et al. Silent venous thromboembolism before treatment in endometrial cancer and the risk factors. Br J Cancer. 2008; 99:1034–1039.11. Satoh T, Oki A, Uno K, Sakurai M, Ochi H, Okada S, et al. High incidence of silent venous thromboembolism before treatment in ovarian cancer. Br J Cancer. 2007; 97:1053–1057.12. Takeshima N, Hirai Y, Umayahara K, Fujiwara K, Takizawa K, Hasumi K. Lymph node metastasis in ovarian cancer: difference between serous and non-serous primary tumors. Gynecol Oncol. 2005; 99:427–431.13. McMurrich JP. The occurrence of congenital adhesions in the common iliac veins and their relation to thrombosis of the femoral and iliac veins. Am J Med Sci. 1908; 135:342–346.14. Ehrich WE, Krumbhaar EB. A frequent obstructive anomaly of the mouth of the left common iliac vein. Am Heart J. 1943; 26:737–750.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Laparoscopic pelvic and para-aortic lymphadenectomy
- Analysis of para-aortic lymphadenectomy up to the level of the renal vessels in apparent early-stage ovarian cancer
- Single-port laparoscopic transperitoneal infrarenal para-aortic lymphadenectomy as part of staging operation for early ovarian cancer and high grade endometrial cancer
- Transperitoneal para-aortic lymphadenectomy by robot assisted laparoscopy in 10 steps
- The Role of the Para-aortic Lymphadenectomy in Epithelial Ovarian Cancer