J Gynecol Oncol.
2014 Jan;25(1):30-35. 10.3802/jgo.2014.25.1.30.
FIGO 1988 versus 2009 staging for endometrial carcinoma: a comparative study on prediction of survival and stage distribution according to histologic subtype
- Affiliations
-
- 1Department of Obstetrics and Gynecology, Helsinki University Central Hospital, Helsinki, Finland. ulla-maija.haltia@fimnet.fi
- 2Department of Pathology, Helsinki University Central Hospital, Helsinki, Finland.
- KMID: 1811185
- DOI: http://doi.org/10.3802/jgo.2014.25.1.30
Abstract
OBJECTIVE
The surgical staging system for endometrial carcinoma developed by International Federation of Gynecology and Obstetrics (FIGO) in 1988 was revised in 2009. Given the importance of continuous validation of the prognostic performance of staging systems, we analyzed the disease specific survival for patients with endometrial carcinoma using FIGO 1988 and 2009 systems. Further, the stage distribution of endometrioid and nonendometrioid carcinomas was studied.
METHODS
Eight hundred twenty-one women with endometrial carcinoma were retrospectively staged using FIGO 1988 and 2009 systems.
RESULTS
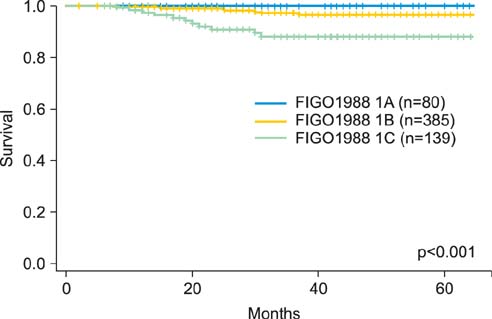
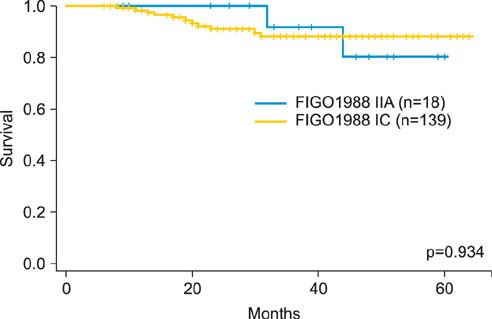
FIGO 1988 IC was associated with an inferior survival compared with IA-IB. Survival overlapped for 1988 IA and IB, for 1988 IC and IIA, and for 2009 IB and II. FIGO 2009 IA-II patients with negative peritoneal cytology had a superior survival compared with 1988 IIIA patients with positive cytology only. The survival was similar for 1988 IIIA with positive cytology only and for 2009 IIIA. Cox proportional hazards model recognized grade 3 endometrioid and nonendometrioid histology, tumor spread beyond the uterine corpus and cervix, and positive peritoneal cytology as significant predictors of death. Among 2009 IIIC substages, the proportion of IIIC2 tumors was higher for nonendometrioid than for endometrioid carcinomas (p=0.003).
CONCLUSION
Stage I with deep myometrial invasion and stage II endometrial carcinoma seem to have similar survival outcomes. Although positive peritoneal cytology does not alter the stage according to the FIGO 2009 system, it should be considered a poor prognostic sign. The high proportion of nonendometrioid carcinomas in the stage IIIC2 category may reflect different patterns of retroperitoneal spread among tumors with different histologic subtypes.
Keyword
MeSH Terms
Figure
Reference
-
1. Siegel R, Naishadham D, Jemal A. Cancer statistics, 2012. CA Cancer J Clin. 2012; 62:10–29.2. Institute for Statistical and Epidemiological Cancer Research. Finnish Cancer Registry: statistics [Internet]. Institute for Statistical and Epidemiological Cancer Research;cited 2013 Nov 20. Available from: http://www.cancerregistry.fi.3. Sorosky JI. Endometrial cancer. Obstet Gynecol. 2012; 120(2 Pt 1):383–397.4. Prat J. Prognostic parameters of endometrial carcinoma. Hum Pathol. 2004; 35:649–662.5. Odicino F, Pecorelli S, Zigliani L, Creasman WT. History of the FIGO cancer staging system. Int J Gynaecol Obstet. 2008; 101:205–210.6. Shepherd JH. Revised FIGO staging for gynaecological cancer. Br J Obstet Gynaecol. 1989; 96:889–892.7. Pecorelli S. Revised FIGO staging for carcinoma of the vulva, cervix, and endometrium. Int J Gynaecol Obstet. 2009; 105:103–104.8. Lewin SN, Herzog TJ, Barrena Medel NI, Deutsch I, Burke WM, Sun X, et al. Comparative performance of the 2009 international Federation of gynecology and obstetrics' staging system for uterine corpus cancer. Obstet Gynecol. 2010; 116:1141–1149.9. Cooke EW, Pappas L, Gaffney DK. Does the revised International Federation of Gynecology and Obstetrics staging system for endometrial cancer lead to increased discrimination in patient outcomes? Cancer. 2011; 117:4231–4237.10. Werner HM, Trovik J, Marcickiewicz J, Tingulstad S, Staff AC, Amant F, et al. Revision of FIGO surgical staging in 2009 for endometrial cancer validates to improve risk stratification. Gynecol Oncol. 2012; 125:103–108.11. Page BR, Pappas L, Cooke EW, Gaffney DK. Does the FIGO 2009 endometrial cancer staging system more accurately correlate with clinical outcome in different histologies? Revised staging, endometrial cancer, histology. Int J Gynecol Cancer. 2012; 22:593–598.12. Kim HJ, Kim TJ, Lee YY, Choi CH, Lee JW, Bae DS, et al. A comparison of uterine papillary serous, clear cell carcinomas, and grade 3 endometrioid corpus cancers using 2009 FIGO staging system. J Gynecol Oncol. 2013; 24:120–127.13. Abu-Rustum NR, Zhou Q, Iasonos A, Alektiar KM, Leitao MM Jr, Chi DS, et al. The revised 2009 FIGO staging system for endometrial cancer: should the 1988 FIGO stages IA and IB be altered? Int J Gynecol Cancer. 2011; 21:511–516.14. Kato T, Watari H, Endo D, Mitamura T, Odagiri T, Konno Y, et al. New revised FIGO 2008 staging system for endometrial cancer produces better discrimination in survival compared with the 1988 staging system. J Surg Oncol. 2012; 106:938–941.15. Kasamatsu T, Onda T, Katsumata N, Sawada M, Yamada T, Tsunematsu R, et al. Prognostic significance of positive peritoneal cytology in endometrial carcinoma confined to the uterus. Br J Cancer. 2003; 88:245–250.16. Tebeu PM, Popowski GY, Verkooijen HM, Casals J, Ludicke F, Zeciri G, et al. Impact of peritoneal cytology on survival of endometrial cancer patients treated with surgery and radiotherapy. Br J Cancer. 2003; 89:2023–2026.17. Fadare O, Mariappan MR, Hileeto D, Wang S, McAlpine JN, Rimm DL. Upstaging based solely on positive peritoneal washing does not affect outcome in endometrial cancer. Mod Pathol. 2005; 18:673–680.18. Takeshima N, Nishida H, Tabata T, Hirai Y, Hasumi K. Positive peritoneal cytology in endometrial cancer: enhancement of other prognostic indicators. Gynecol Oncol. 2001; 82:470–473.19. Mariani A, Webb MJ, Keeney GL, Aletti G, Podratz KC. Assessment of prognostic factors in stage IIIA endometrial cancer. Gynecol Oncol. 2002; 86:38–44.20. Garg G, Gao F, Wright JD, Hagemann AR, Mutch DG, Powell MA. Positive peritoneal cytology is an independent risk-factor in early stage endometrial cancer. Gynecol Oncol. 2013; 128:77–82.21. Zaino RJ, Abendroth C, Yemelyanova A, Oliva E, Lim D, Soslow R, et al. Endocervical involvement in endometrial adenocarcinoma is not prognostically significant and the pathologic assessment of the pattern of involvement is not reproducible. Gynecol Oncol. 2013; 128:83–87.22. Hamilton CA, Cheung MK, Osann K, Chen L, Teng NN, Longacre TA, et al. Uterine papillary serous and clear cell carcinomas predict for poorer survival compared to grade 3 endometrioid corpus cancers. Br J Cancer. 2006; 94:642–646.23. Guntupalli SR, Zighelboim I, Kizer NT, Zhang Q, Powell MA, Thaker PH, et al. Lymphovascular space invasion is an independent risk factor for nodal disease and poor outcomes in endometrioid endometrial cancer. Gynecol Oncol. 2012; 124:31–35.24. Salvesen HB, Haldorsen IS, Trovik J. Markers for individualised therapy in endometrial carcinoma. Lancet Oncol. 2012; 13:e353–e361.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A comparison of uterine papillary serous, clear cell carcinomas, and grade 3 endometrioid corpus cancers using 2009 FIGO staging system
- The Clinical Analysis of Endometrial Cancer by Surgical Staging
- 3 Cases of Synchronous Primary Carcinomas
- FIGO Staging for Uterine Sarcomas: Can the Revised 2008 Staging System Predict Survival Outcome Better?
- The Clinical Analysis of Endometrial Cancer by Surgical Staging