J Cerebrovasc Endovasc Neurosurg.
2012 Sep;14(3):251-254. 10.7461/jcen.2012.14.3.251.
The Role of Hyperthyroidism as the Predisposing Factor for Superior Sagittal Sinus Thrombosis
- Affiliations
-
- 1Department of Neurosurgery, Cheongju St. Mary's Hospital, Cheongju, Korea. drkwon72@naver.com
- KMID: 1808465
- DOI: http://doi.org/10.7461/jcen.2012.14.3.251
Abstract
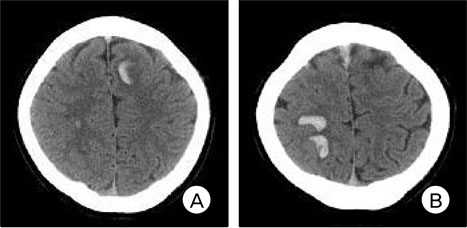
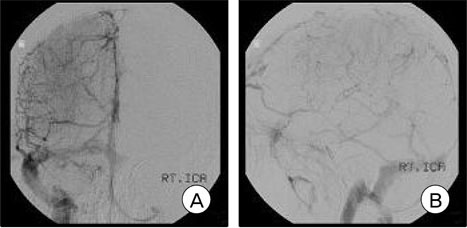
- Superior sagittal sinus thrombosis (SSST) is an uncommon cause of stroke, whose symptoms and clinical course are highly variable. It is frequently associated with a variety of hypercoagulable states. Coagulation abnormalities are commonly seen in patients with hyperthyroidism. To the best of our knowledge, there are few reports on the association between hyperthyroidism and cerebral venous thrombosis. We report on a 31-year-old male patient with a six-year history of hyperthyroidism who developed seizure and mental deterioration. Findings on brain computed tomography (CT) showed multiple hemorrhages in the subcortical area of both middle frontal gyrus and cerebral digital subtraction angiography (DSA) showed irregular intra-luminal filling defects of the superior sagittal sinus. These findings were consistent with hemorrhagic transformation of SSST. Findings on clinical laboratory tests were consistent with hyperthyroidism. In addition, our patient also showed high activity of factors IX and XI. The patient received treatment with oral anticoagulant and prophylthiouracil. His symptoms showed complete improvement. A follow-up cerebral angiography four weeks after treatment showed a recanalization of the SSS. In conclusion, findings of our case indicate that hypercoagulability may contribute to development of SSST in a patient with hyperthyroidism.
MeSH Terms
Figure
Cited by 1 articles
-
Massive cerebral venous sinus thrombosis secondary to Graves' disease
Hye-Min Son
Yeungnam Univ J Med. 2019;36(3):273-280. doi: 10.12701/yujm.2019.00339.
Reference
-
1. Ameri A, Bousser MG. Cerebral venous thrombosis. Neurol Clin. 1992. 02. 10(1):87–111.
Article2. Bar-Sela S, Ehrenfeld M, Eliakim M. Arterial embolism in thyrotoxicosis with atrial fibrillation. Arch Intern Med. 1981. 08. 141(9):1191–1192.
Article3. Chang DC, Wheeler MH, Woodcock JP, Curley I, Lazarus JR, Fung H, et al. The effect of preoperative Lugol's iodine on thyroid blood flow in patients with Graves' hyperthyroidism. Surgery. 1987. 12. 102(6):1055–1061.4. Dai A, Wasay M, Dubey N, Giglio P, Bakshi R. Superior sagittal sinus thrombosis secondary to hyperthyroidism. J Stroke Cerebrovasc Dis. 2000. Mar-Apr. 9(2):89–90.
Article5. de Bruijn SF, de Haan RJ, Stam J. For the Cerebral Venous Sinus Thrombosis Study Group. Clinical features and prognostic factors of cerebral venous thrombosis in a prospective series of 59 patients. J Neurol Neurosurg Psychiatry. 2001. 01. 70(1):105–108.6. Egeberg O. Influence of thyroid function on the blood clotting system. Scand J Clin Lab Invest. 1963. 15(1):1–7.
Article7. Einhäupl K, Bousser MG, de Bruijn SF, Ferro JM, Martinelli I, Masuhr F, et al. EFNS guideline on the treatment of cerebral venous and sinus thrombosis. Eur J Neurol. 2006. 06. 13(6):553–559.
Article8. Ferro JM, Canhão P, Stam J, Bousser MG, Barinagarrementeria F. ISCVT Investigators. Prognosis of cerebral vein and dural sinus thrombosis: Results of the International Study on Cerebral Vein and Dural Sinus Thrombosis (ISCVT). Stroke. 2004. 03. 35(3):664–667.9. Farid NR, Griffiths BL, Collins JR, Marshall WH, Ingram DW. Blood coagulation and fibrinolysis in thyroid disease. Thromb Haemost. 1976. 04. 35(2):415–422.
Article10. Hodgson KJ, Lazarus JH, Wheeler MH, Woodcock JP, Owen GM, McGregor AM, et al. Duplex scan-derived thyroid blood flow in euthyroid and hyperthyroid patients. World J Surg. 1988. 08. 12(4):470–475.
Article11. Hurley DM, Hunter AN, Hewett MJ, Stockigt JR. Atrial fibrillation and arterial embolism in hyperthyroidism. Aust N Z J Med. 1981. 08. 11(4):391–393.
Article12. Meijers JC, Tekelenburg WL, Bouma BN, Bertina RM, Rosendaal FR. High levels of coagulation factor XI as a risk factor for venous thrombosis. N Engl J Med. 2000. 03. 342(10):696–701.
Article13. Petersen P, Hansen JM. Stroke in thyrotoxicosis with atrial fibrillation. Stroke. 1988. 01. 19(1):15–18.
Article14. Prentice CRM, Forbes CD, Smith SM. Rise of factor VIII activity after exercise and adrenaline infusion, measured by immunological and biological techniques. Thromb Res. 1972. 10. 1(5):493–505.15. Rogers JS 2nd, Shane SR, Jencks FS. Factor VIII activity and thyroid function. Ann Intern Med. 1982. 11. 97(5):713–716.
Article16. Schutta HS, Williams EC, Baranski BG, Sutula TP. Cerebral venous thrombosis with plasminogen deficiency. Stroke. 1991. 03. 22(3):401–405.
Article17. Siegert CE, Smelt AH, de Bruin TW. Superior sagittal thrombosis and thyrotoxicosis. Possible association in two cases. Stroke. 1995. 03. 26(3):496–497.18. Simone JV, Abildgaard CF, Schulman I. Blood coagulation in thyroid dysfunction. N Engl J Med. 1965. 11. 273(20):1057–1061.
Article19. Stam J. Thrombosis of the cerebral veins and sinuses. N Engl J Med. 2005. 04. 352(17):1791–1798.
Article20. van Hylckama Vlieg A, van der Linden IK, Bertina RM, Rosendaal FR. High levels of factor XI increase the risk of venous thrombosis. Blood. 2000. 06. 95(12):3678–3682.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Cerebral Venous Thrombosis in a Patient with Graves' Disease
- A Case of Eosinophilic Panniculitis Associated With Superior Sagittal Sinus Thrombosis
- Thrombosis of the Superior Sagittal Sinus in Behcet's Disease With Vascular and Enteric Involvements
- Cerebral Venous Sinus Thrombosis in an Adolescent Presenting with Headache
- Superior sagittal sinus dural arteriovenous fistula caused by treatment of meningioma masquerades as sinus thrombosis