J Cardiovasc Ultrasound.
2015 Jun;23(2):86-90. 10.4250/jcu.2015.23.2.86.
Excessive Weight and Obesity Are Associated to Intra-Ventricular Asynchrony: Pilot Study
- Affiliations
-
- 1Department of Echocardiography, "Ignacio Chavez" National Cardiology Institute, Mexico City, Mexico. vazzny74@yahoo.com
- 2Intermediate Care, Clinical Foundation Medica Sur, Mexico City, Mexico.
- KMID: 1806916
- DOI: http://doi.org/10.4250/jcu.2015.23.2.86
Abstract
- BACKGROUND
Excessive weight and obesity (EwO) are independent factors in the development of heart failure; they lead to a state of myocardiopathy via inflammatory and hormonal mechanisms. If excessively accumulated, epicardial fat favors a proinflammatory state. Ventricular asynchrony is a marker of heart failure progression and has been poorly studied in EwO. The objective was evaluate the relation between epicardial fat, body mass index (BMI) and mechanical synchrony measured by echocardiography, in healthy individuals with EwO.
METHODS
We included 55 healthy individuals between the ages of 18 and 35, 17 had a BMI < 25 kg/m2 (30.9%) and 38 had a BMI > 25 kg/m2 (EwO group) (69.09%), anthropometric measurements, transthoracic echocardiogram and synchrony evaluation were obtained.
RESULTS
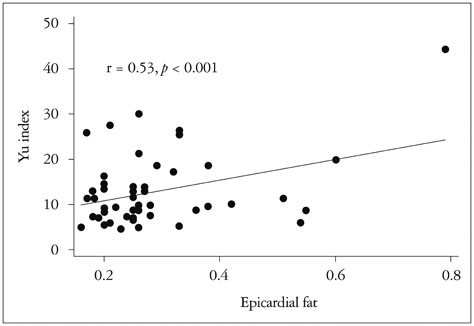
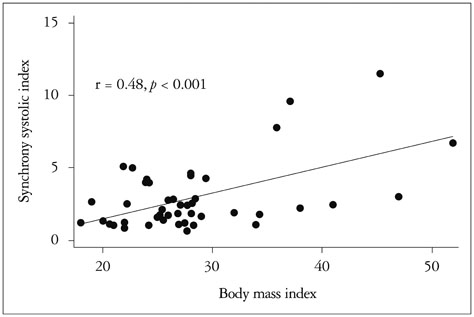
Left atrial volume, telediastolic and telesystolic left ventricular volumes and the baseline volume of the right ventricle were greater in the EwO group (20 mL/m2 vs. 15 mL/m2, p = 0.001; 106 mL vs. 82 mL, p = 0.0149 vs. 32 mL, p = 0.001 and 34 mm vs. 31 mm, p = 0.02, respectively). The Yu index also correlated with epicardial fat, r = 0.53, p < 0.01, whereby the greater the amount of epicardial fat, the greater the dispersion timing of ventricular activation. The systolic synchrony index also correlated with the BMI, p = 0.01.
CONCLUSION
Mechanical intraventricular asynchrony is associated to EwO and the amount of epicardial fat; hence, asynchrony may be one more factor leading to heart failure in EwO individuals.
MeSH Terms
Figure
Reference
-
1. Mokdad AH, Serdula MK, Dietz WH, Bowman BA, Marks JS, Koplan JP. The spread of the obesity epidemic in the United States, 1991-1998. JAMA. 1999; 282:1519–1522.2. Barquera S, Campos-Nonato I, Hernández-Barrera L, Pedroza A, Rivera-Dommarco JA. [Prevalence of obesity in Mexican adults 2000-2012]. Salud Publica Mex. 2013; 55:Suppl 2. S151–S160.3. Hubert HB, Feinleib M, McNamara PM, Castelli WP. Obesity as an independent risk factor for cardiovascular disease: a 26-year follow-up of participants in the Framingham Heart Study. Circulation. 1983; 67:968–977.4. Chen YT, Vaccarino V, Williams CS, Butler J, Berkman LF, Krumholz HM. Risk factors for heart failure in the elderly: a prospective community-based study. Am J Med. 1999; 106:605–612.5. Murphy NF, MacIntyre K, Stewart S, Hart CL, Hole D, McMurray JJ. Long-term cardiovascular consequences of obesity: 20-year follow-up of more than 15 000 middle-aged men and women (the Renfrew-Paisley study). Eur Heart J. 2006; 27:96–106.6. Ritchie RH. Evidence for a causal role of oxidative stress in the myocardial complications of insulin resistance. Heart Lung Circ. 2009; 18:11–18.7. Iozzo P. Myocardial, perivascular, and epicardial fat. Diabetes Care. 2011; 34:Suppl 2. S371–S379.8. Alpert MA. Obesity cardiomyopathy: pathophysiology and evolution of the clinical syndrome. Am J Med Sci. 2001; 321:225–236.9. Kass DA. An epidemic of dyssynchrony: but what does it mean? J Am Coll Cardiol. 2008; 51:12–17.10. Korosoglou G, Humpert PM, Halbgewachs E, Bekeredjian R, Filusch A, Buss SJ, Morcos M, Bierhaus A, Katus HA, Nawroth PP, Kuecherer H. Evidence of left ventricular contractile asynchrony by echocardiographic phase imaging in patients with type 2 diabetes mellitus and without clinically evident heart disease. Am J Cardiol. 2006; 98:1525–1530.11. Schuster I, Vinet A, Karpoff L, Startun A, Jourdan N, Dauzat M, Nottin S, Perez-Martin A. Diastolic dysfunction and intraventricular dyssynchrony are restored by low intensity exercise training in obese men. Obesity (Silver Spring). 2012; 20:134–140.12. Gorcsan J 3rd, Abraham T, Agler DA, Bax JJ, Derumeaux G, Grimm RA, Martin R, Steinberg JS, Sutton MS, Yu CM. American Society of Echocardiography Dyssynchrony Writing Group. Echocardiography for cardiac resynchronization therapy: recommendations for performance and reporting--a report from the American Society of Echocardiography Dyssynchrony Writing Group endorsed by the Heart Rhythm Society. J Am Soc Echocardiogr. 2008; 21:191–213.13. Iacobellis G, Willens HJ. Echocardiographic epicardial fat: a review of research and clinical applications. J Am Soc Echocardiogr. 2009; 22:1311–1319. quiz 1417-814. Lang RM, Bierig M, Devereux RB, Flachskampf FA, Foster E, Pellikka PA, Picard MH, Roman MJ, Seward J, Shanewise JS, Solomon SD, Spencer KT, Sutton MS, Stewart WJ. Chamber Quantification Writing Group. American Society of Echocardiography's Guidelines and Standards Committee. European Association of Echocardiography. Recommendations for chamber quantification: a report from the American Society of Echocardiography's Guidelines and Standards Committee and the Chamber Quantification Writing Group, developed in conjunction with the European Association of Echocardiography, a branch of the European Society of Cardiology. J Am Soc Echocardiogr. 2005; 18:1440–1463.15. Mor-Avi V, Lang RM, Badano LP, Belohlavek M, Cardim NM, Derumeaux G, Galderisi M, Marwick T, Nagueh SF, Sengupta PP, Sicari R, Smiseth OA, Smulevitz B, Takeuchi M, Thomas JD, Vannan M, Voigt JU, Zamorano JL. Current and evolving echocardiographic techniques for the quantitative evaluation of cardiac mechanics: ASE/EAE consensus statement on methodology and indications endorsed by the Japanese Society of Echocardiography. Eur J Echocardiogr. 2011; 12:167–205.16. Yu CM, Fung WH, Lin H, Zhang Q, Sanderson JE, Lau CP. Predictors of left ventricular reverse remodeling after cardiac resynchronization therapy for heart failure secondary to idiopathic dilated or ischemic cardiomyopathy. Am J Cardiol. 2003; 91:684–688.17. Marfella R, Esposito K, Siniscalchi M, Cacciapuoti F, Giugliano F, Labriola D, Ciotola M, Di Palo C, Misso L, Giugliano D. Effect of weight loss on cardiac synchronization and proinflammatory cytokines in premenopausal obese women. Diabetes Care. 2004; 27:47–52.18. Delcour KS, Tejwani L, Hayden MR, Govindarajan G. Intraventricular mechanical asynchrony in asymptomatic morbidly obese individuals. J Cardiometab Syndr. 2007; 2:305–308.19. Kramer SP, Powell DK, Haggerty CM, Binkley CM, Mattingly AC, Cassis LA, Epstein FH, Fornwalt BK. Obesity reduces left ventricular strains, torsion, and synchrony in mouse models: a cine displacement encoding with stimulated echoes (DENSE) cardiovascular magnetic resonance study. J Cardiovasc Magn Reson. 2013; 15:109.20. Grines CL, Bashore TM, Boudoulas H, Olson S, Shafer P, Wooley CF. Functional abnormalities in isolated left bundle branch block. The effect of interventricular asynchrony. Circulation. 1989; 79:845–853.21. Zhou YT, Grayburn P, Karim A, Shimabukuro M, Higa M, Baetens D, Orci L, Unger RH. Lipotoxic heart disease in obese rats: implications for human obesity. Proc Natl Acad Sci U S A. 2000; 97:1784–1789.22. Chiu HC, Kovacs A, Ford DA, Hsu FF, Garcia R, Herrero P, Saffitz JE, Schaffer JE. A novel mouse model of lipotoxic cardiomyopathy. J Clin Invest. 2001; 107:813–822.23. Sharma S, Adrogue JV, Golfman L, Uray I, Lemm J, Youker K, Noon GP, Frazier OH, Taegtmeyer H. Intramyocardial lipid accumulation in the failing human heart resembles the lipotoxic rat heart. FASEB J. 2004; 18:1692–1700.24. Szczepaniak LS, Dobbins RL, Metzger GJ, Sartoni-D'Ambrosia G, Arbique D, Vongpatanasin W, Unger R, Victor RG. Myocardial triglycerides and systolic function in humans: in vivo evaluation by localized proton spectroscopy and cardiac imaging. Magn Reson Med. 2003; 49:417–423.25. Iozzo P, Lautamaki R, Borra R, Lehto HR, Bucci M, Viljanen A, Parkka J, Lepomaki V, Maggio R, Parkkola R, Knuuti J, Nuutila P. Contribution of glucose tolerance and gender to cardiac adiposity. J Clin Endocrinol Metab. 2009; 94:4472–4482.26. Messerli FH, Ventura HO, Reisin E, Dreslinski GR, Dunn FG, MacPhee AA, Frohlich ED. Borderline hypertension and obesity: two prehypertensive states with elevated cardiac output. Circulation. 1982; 66:55–60.27. Peterson LR, Waggoner AD, Schechtman KB, Meyer T, Gropler RJ, Barzilai B, Dávila-Román VG. Alterations in left ventricular structure and function in young healthy obese women: assessment by echocardiography and tissue Doppler imaging. J Am Coll Cardiol. 2004; 43:1399–1404.28. Krishnan R, Becker RJ, Beighley LM, López-Candales A. Impact of body mass index on markers of left ventricular thickness and mass calculation: results of a pilot analysis. Echocardiography. 2005; 22:203–210.29. Di Salvo G, Pacileo G, Del Giudice EM, Natale F, Limongelli G, Verrengia M, Rea A, Fratta F, Castaldi B, D'Andrea A, Calabrò P, Miele T, Coppola F, Russo MG, Caso P, Perrone L, Calabrò R. Abnormal myocardial deformation properties in obese, non-hypertensive children: an ambulatory blood pressure monitoring, standard echocardiographic, and strain rate imaging study. Eur Heart J. 2006; 27:2689–2695.30. Wierzbowska-Drabik K, Chrzanowski L, Kapusta A, Uznańska-Loch B, Płońska E, Krzemińska-Pakuła M, Kurpesa M, Rechciński T, Trzos E, Kasprzak JD. Severe obesity impairs systolic and diastolic heart function - the significance of pulsed tissue Doppler, strain, and strain rate parameters. Echocardiography. 2013; 30:904–911.31. Wong C, Marwick TH. Obesity cardiomyopathy: pathogenesis and pathophysiology. Nat Clin Pract Cardiovasc Med. 2007; 4:436–443.32. Malavazos AE, Corsi MM, Ermetici F, Coman C, Sardanelli F, Rossi A, Morricone L, Ambrosi B. Proinflammatory cytokines and cardiac abnormalities in uncomplicated obesity: relationship with abdominal fat deposition. Nutr Metab Cardiovasc Dis. 2007; 17:294–302.