Ann Surg Treat Res.
2014 Jul;87(1):47-50. 10.4174/astr.2014.87.1.47.
The paracholedochal vein: a feasible option as portal inflow in living donor liver transplantation
- Affiliations
-
- 1Division of Hepatobiliary Pancreas Surgery and Abdominal Organ Transplantation, Department of Surgery, Daegu Catholic University School of Medicine, Daegu, Korea. dnchoi@cu.ac.kr
- KMID: 1804100
- DOI: http://doi.org/10.4174/astr.2014.87.1.47
Abstract
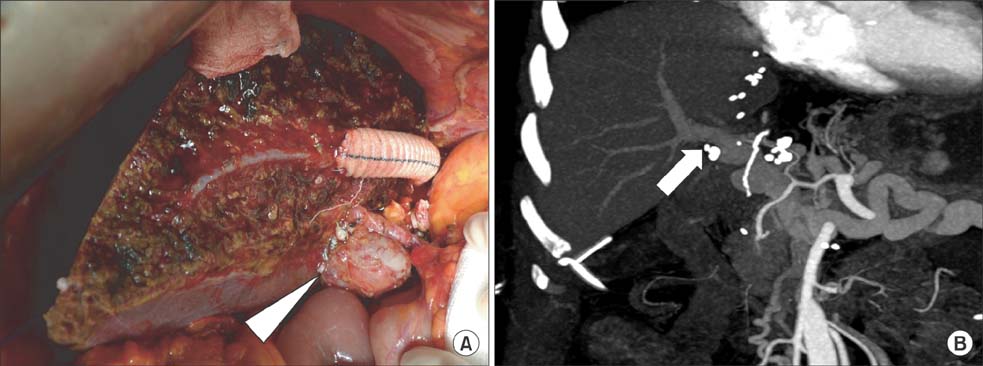
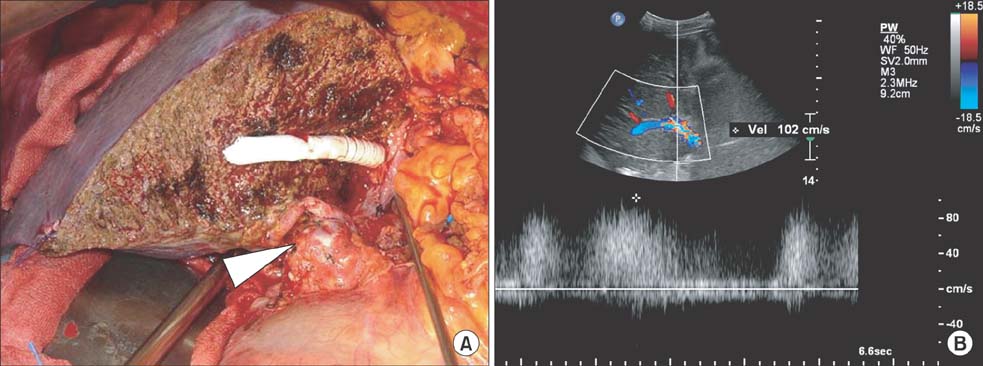
- Extensive thrombosis of the portal and splenomesenteric veins combined with cavernous transformation of the portal vein (CTPV) has been considered to be a contraindication for living donor liver transplantation (LDLT) due to technical difficulties and perioperative risks. In recent years, several surgical innovations including cavoportal hemitransposition, renoportal anastomosis, and portal arterialization have been introduced to overcome diffuse portal vein thrombosis (PVT) and CTPV, but their outcomes were unsatisfactory with significant morbidity and mortality. Herein, we report two successful cases of adult LDLT in diffuse PVT with CTPV managed using the paracholedochal vein as portal inflow to the graft.
MeSH Terms
Figure
Reference
-
1. Maluf D, Shim I, Posner M, Cotterell AH, Fisher RA. Salvage procedure for unexpected portal vein thrombosis in living donor liver transplantation. Transplant Proc. 2006; 38:1422–1424.2. Rotellar F, Cienfuegos JA, Bueno A, Marti P, Valenti V, Zozaya G, et al. Portal revascularization in the setting of cavernous transformation through a paracholedocal vein: a case report. Transplant Proc. 2010; 42:3079–3080.3. Paskonis M, Jurgaitis J, Mehrabi A, Kashfi A, Fonouni H, Strupas K, et al. Surgical strategies for liver transplantation in the case of portal vein thrombosis: current role of cavoportal hemitransposition and renoportal anastomosis. Clin Transplant. 2006; 20:551–562.4. Zhang MM, Jin XQ, Yan LN, Kang Q, Guo CB. Living-related liver transplantation for cavernous transformation of portal vein: a clinical study of 3 cases. Zhonghua Gan Zang Bing Za Zhi. 2008; 16:270–273.5. Zhang M, Guo C, Pu C, Ren Z, Li Y, Kang Q, et al. Adult to pediatric living donor liver transplantation for portal cavernoma. Hepatol Res. 2009; 39:888–897.6. Tao YF, Teng F, Wang ZX, Guo WY, Shi XM, Wang GH, et al. Liver transplant recipients with portal vein thrombosis: a single center retrospective study. Hepatobiliary Pancreat Dis Int. 2009; 8:34–39.7. Cho JY, Suh KS, Shin WY, Lee HW, Yi NJ, Lee KU. Thrombosis confined to the portal vein is not a contraindication for living donor liver transplantation. World J Surg. 2008; 32:1731–1737.8. Zhang LJ, Yang GF, Jiang B, Wen LQ, Shen W, Qi J. Cavernous transformation of portal vein: 16-slice CT portography and correlation with surgical procedure of orthotopic liver transplantation. Abdom Imaging. 2008; 33:529–535.9. Hiatt JR, Quinones-Baldrich WJ, Ramming KP, Lois JF, Busuttil RW. Bile duct varices. An alternative to portoportal anastomosis in liver transplantation. Transplantation. 1986; 42:85.10. Wu TH, Chou HS, Pan KT, Lee CS, Wu TJ, Chu SY, et al. Application of cryopreserved vein grafts as a conduit between the coronary vein and liver graft to reconstruct portal flow in adult living liver transplantation. Clin Transplant. 2009; 23:751–755.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Portal vein fenestration: a case report of an unusual portal vein developmental anomaly
- Portal flow augmentation using meso-reno-portal anastomosis during liver transplantation with severe portal vein thrombosis
- Portal vein interposition in living donor liver transplantation for a pediatric hepatoblastoma patient with portal vein tumor thrombosis
- Lessons Learned from Inappropriate Ligation of the Left Renal Vein for a Large Splenorenal Shunt in Living Donor Liver Transplantation
- Successful laparoscopic living donor right hepatectomy in a case with challenging portal vein variation