Korean J Hepatobiliary Pancreat Surg.
2015 Feb;19(1):6-10. 10.14701/kjhbps.2015.19.1.6.
Gallbladder perforation: a single center experience of 32 cases
- Affiliations
-
- 1Department of Surgery, Vardhman Mahavir Medical College and Safdarjung Hospital, New Delhi, India. debasismbbs@gmail.com
- KMID: 1802233
- DOI: http://doi.org/10.14701/kjhbps.2015.19.1.6
Abstract
- BACKGROUNDS/AIMS
Gallbladder perforation is a rare but potentially fatal disease. We herein present our clinical experience in diagnosis and management of 32 cases of gallbladder perforation.
METHODS
This retrospective study was conducted with inclusion of all cases of gallbladder perforation that presented to our hospital from January 2012 to November 2014. Cases of traumatic gallbladder perforation and patients younger than 12 years of age were excluded from this study.
RESULTS
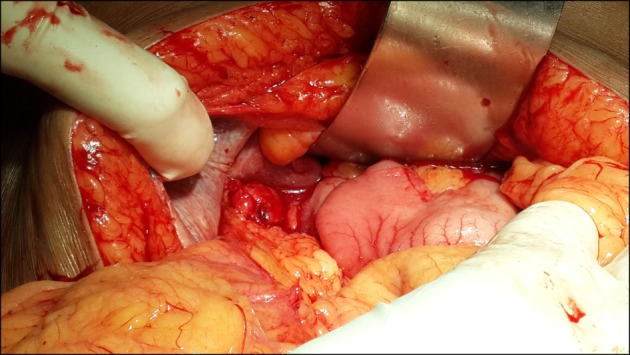
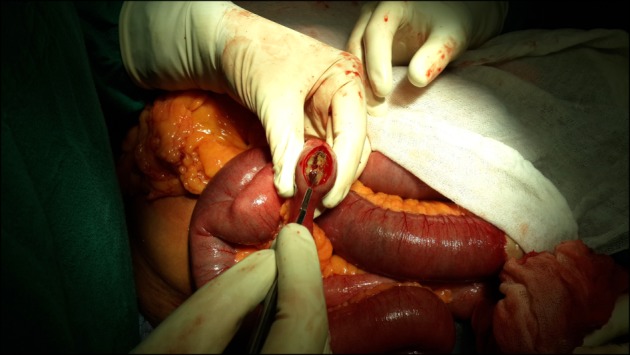
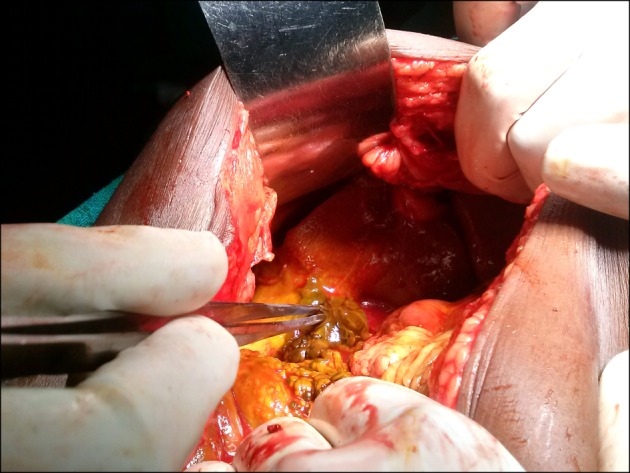
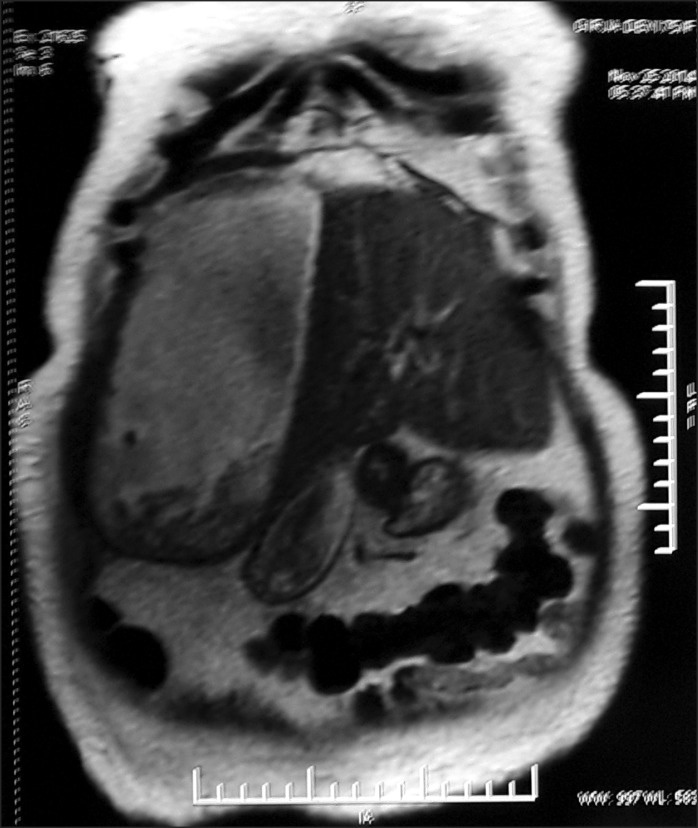
This study included 32 patients (13 males and 19 females). The mean age of patients was 55.9 years. Gallbladder perforation was most common in the 5th and 6th decade of life. The mean age of patients with type I, II, and III gallbladder perforation was 57.0 years, 57.6 years, and 49.8 years, respectively. The most common site of perforation was the fundus, followed by the body and Hartmann's pouch (24 : 5 : 2). Most of the type I gallbladder perforations were diagnosed intraoperatively, type II gallbladder perforations were diagnosed by enhanced abdominal computed tomography, and type III gallbladder perforations were diagnosed during laparoscopic cholecystectomy converted to open cholecystectomy for cholelithiasis. Mortality was highest in patients with type I gallbladder perforation. The mean hospital stay was 10.1 days, 6.4 days, and 9.2 days in patients with type I, II, and III gallbladder perforation, respectively. The histopathologic analysis in 28 patients who were operated on showed acute cholecystitis in 19 cases, acute-on-chronic cholecystitis in 4 cases, chronic cholecystitis in 4 cases, and mucinous adenocarcinoma of the gallbladder in a single case.
CONCLUSIONS
Gallbladder perforation represents a special diagnostic and surgical challenge. Appropriate classification and management are essential.
Keyword
MeSH Terms
Figure
Reference
-
1. Khan SA, Gulfam , Anwer AW, Arshad Z, Hameed K, Shoaib M. Gallbladder perforation: a rare complication of acute cholecystitis. J Pak Med Assoc. 2010; 60:228–229. PMID: 20225785.2. Teefey SA, Wechter DG. Sonographic evaluation of pericholecystic abscess with intrahepatic extension. J Ultrasound Med. 1987; 6:659–662. PMID: 3682057.
Article3. Niemeier OW. Acute free perforation of the gall-bladder. Ann Surg. 1934; 99:922–924. PMID: 17867204.
Article4. Simmons TC, Miller C, Weaver R. Spontaneous gallbladder perforation. Am Surg. 1989; 55:311–313. PMID: 2655511.5. Aljiffry M, Walsh M, Peltekian K, Molinari M. Type II gall bladder perforation with abdominal wall abscess in a cirrhotic patient: case report and review of the literature. J Surg Educ. 2008; 65:367–371. PMID: 18809168.
Article6. Alvi AR, Ajmal S, Saleem T. Acute free perforation of gall bladder encountered at initial presentation in a 51 years old man: A case report. Cases J. 2009; 2:166. PMID: 19946477.
Article7. Sood BP, Kalra N, Gupta S, Sidhu R, Gulati M, Khandelwal N, et al. Role of sonography in the diagnosis of gallbladder perforation. J Clin Ultrasound. 2002; 30:270–274. PMID: 12116106.
Article8. Derici H, Kara C, Bozdag AD, Nazli O, Tansug T, Akca E. Diagnosis and treatment of gallbladder perforation. World J Gastroenterol. 2006; 12:7832–7836. PMID: 17203529.9. Karcaaltincaba M, Hohenwalter MD, Erickson SJ, Taylor AJ. MRCP findings of gallbladder perforation and pericholecystic abscess. CMIG Extra: Cases. 2004; 28:59–61.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Iatrogenic Gallbladder Perforation during Gastric Endoscopic Mucosal Resection
- A Case of Spontaneous Gallbladder Perforation
- CT Findings of Gallbladder Perforation
- Gallbladder Perforation after Transarterial Chemoembolization in a Patient with a Huge Hepatocellular Carcinoma
- Gallbladder Perforation without Gallstones or Cholecystitis