Yonsei Med J.
2013 Nov;54(6):1545-1549. 10.3349/ymj.2013.54.6.1545.
Successful Azathioprine Treatment with Metabolite Monitoring in a Pediatric Inflammatory Bowel Disease Patient Homozygous for TPMT*3C
- Affiliations
-
- 1Department of Laboratory Medicine and Genetics, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea. suddenbz@skku.edu
- 2Department of Pediatrics, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea. yonho.choe@samsung.com
- KMID: 1798157
- DOI: http://doi.org/10.3349/ymj.2013.54.6.1545
Abstract
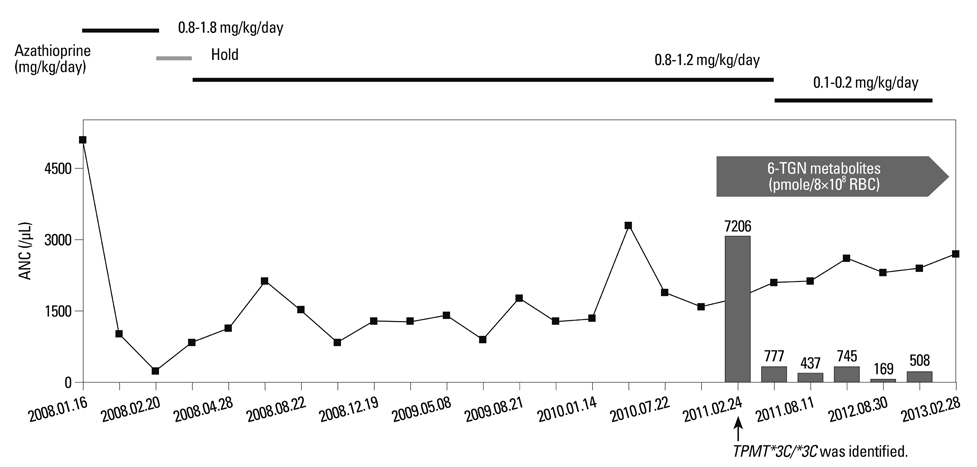
- Thiopurine S-methyltransferase (TPMT) methylates purine analogues, showing TPMT activity in inverse relation to concentrations of active metabolites such as 6-thioguanine nucleotide (6-TGN). With conventional dosing of thiopurines, patients with homozygous variant TPMT alleles consistently suffer from severe myelosuppression. Here, we report a patient with TPMT*3C/*3C who managed successfully with monitoring of thiopurine metabolites. The patient was an 18-year-old male diagnosed with Crohn's disease. The standard dose of azathioprine (AZA) (1.8 mg/kg/day) with mesalazine (55.6 mg/kg/day) was prescribed. Two weeks after starting AZA treatment, the patient developed leukopenia. The DNA sequence analysis of TPMT identified a homozygous missense variation (NM_000367.2: c.719A>G; p.Tyr240Cys), TPMT*3C/*3C. He was treated with adjusted doses of azathioprine (0.1-0.2 mg/kg/day) and his metabolites were closely monitored. Leukopenia did not reoccur during the follow-up period of 24 months. To our knowledge, this is the first case of a patient homozygous for TPMT*3C successfully treated with azathioprine in Korea. While a TPMT genotyping test may be helpful to determine a safe starting dose, it may not completely prevent myelosuppression. Monitoring metabolites as well as routine laboratory tests can contribute to assessing drug metabolism and optimizing drug dosing with minimized drug-induced toxicity.
MeSH Terms
Figure
Reference
-
1. Appell ML, Berg J, Duley J, Evans WE, Kennedy MA, Lennard L, et al. Nomenclature for alleles of the thiopurine methyltransferase gene. Pharmacogenet Genomics. 2013; 23:242–248.
Article2. Krynetski EY, Tai HL, Yates CR, Fessing MY, Loennechen T, Schuetz JD, et al. Genetic polymorphism of thiopurine S-methyl-transferase: clinical importance and molecular mechanisms. Pharmacogenetics. 1996; 6:279–290.
Article3. Tai HL, Krynetski EY, Schuetz EG, Yanishevski Y, Evans WE. Enhanced proteolysis of thiopurine S-methyltransferase (TPMT) encoded by mutant alleles in humans (TPMT*3A, TPMT*2): mechanisms for the genetic polymorphism of TPMT activity. Proc Natl Acad Sci U S A. 1997; 94:6444–6449.
Article4. Tai HL, Krynetski EY, Yates CR, Loennechen T, Fessing MY, Krynetskaia NF, et al. Thiopurine S-methyltransferase deficiency: two nucleotide transitions define the most prevalent mutant allele associated with loss of catalytic activity in Caucasians. Am J Hum Genet. 1996; 58:694–702.5. Hindorf U, Lindqvist M, Hildebrand H, Fagerberg U, Almer S. Adverse events leading to modification of therapy in a large cohort of patients with inflammatory bowel disease. Aliment Pharmacol Ther. 2006; 24:331–342.
Article6. Dewit O, Starkel P, Roblin X. Thiopurine metabolism monitoring: implications in inflammatory bowel diseases. Eur J Clin Invest. 2010; 40:1037–1047.
Article7. Relling MV, Gardner EE, Sandborn WJ, Schmiegelow K, Pui CH, Yee SW, et al. Clinical pharmacogenetics implementation consortium guidelines for thiopurine methyltransferase genotype and thiopurine dosing: 2013 update. Clin Pharmacol Ther. 2013; 93:324–325.
Article8. Dervieux T, Meyer G, Barham R, Matsutani M, Barry M, Boulieu R, et al. Liquid chromatography-tandem mass spectrometry analysis of erythrocyte thiopurine nucleotides and effect of thiopurine methyltransferase gene variants on these metabolites in patients receiving azathioprine/6-mercaptopurine therapy. Clin Chem. 2005; 51:2074–2084.
Article9. Dubinsky MC, Lamothe S, Yang HY, Targan SR, Sinnett D, Théorêt Y, et al. Pharmacogenomics and metabolite measurement for 6-mercaptopurine therapy in inflammatory bowel disease. Gastroenterology. 2000; 118:705–713.
Article10. Cuffari C, Dassopoulos T, Turnbough L, Thompson RE, Bayless TM. Thiopurine methyltransferase activity influences clinical response to azathioprine in inflammatory bowel disease. Clin Gastroenterol Hepatol. 2004; 2:410–417.
Article11. Kumagai K, Hiyama K, Ishioka S, Sato H, Yamanishi Y, McLeod HL, et al. Allelotype frequency of the thiopurine methyltransferase (TPMT) gene in Japanese. Pharmacogenetics. 2001; 11:275–278.
Article12. Kim JH, Cheon JH, Kim WH. [The frequency and the course of the adverse effects of azathioprine/6-mercaptopurine treatment in patients with inflammatory bowel disease]. Korean J Gastroenterol. 2008; 51:291–297.13. Kim JH, Cheon JH, Hong SS, Eun CS, Byeon JS, Hong SY, et al. Influences of thiopurine methyltransferase genotype and activity on thiopurine-induced leukopenia in Korean patients with inflammatory bowel disease: a retrospective cohort study. J Clin Gastroenterol. 2010; 44:e242–e248.14. Lee HJ, Yang SK, Kim KJ, Choe JW, Yoon SM, Ye BD, et al. The safety and efficacy of azathioprine and 6-mercaptopurine in the treatment of Korean patients with Crohn's disease. Intest Res. 2009; 7:22–31.15. Hindorf U, Lindqvist M, Peterson C, Söderkvist P, Ström M, Hjortswang H, et al. Pharmacogenetics during standardised initiation of thiopurine treatment in inflammatory bowel disease. Gut. 2006; 55:1423–1431.
Article16. Gisbert JP, Niño P, Rodrigo L, Cara C, Guijarro LG. Thiopurine methyltransferase (TPMT) activity and adverse effects of azathioprine in inflammatory bowel disease: long-term follow-up study of 394 patients. Am J Gastroenterol. 2006; 101:2769–2776.
Article17. Zelinkova Z, Derijks LJ, Stokkers PC, Vogels EW, van Kampen AH, Curvers WL, et al. Inosine triphosphate pyrophosphatase and thiopurine s-methyltransferase genotypes relationship to azathioprine-induced myelosuppression. Clin Gastroenterol Hepatol. 2006; 4:44–49.
Article18. Colombel JF, Ferrari N, Debuysere H, Marteau P, Gendre JP, Bonaz B, et al. Genotypic analysis of thiopurine S-methyltransferase in patients with Crohn's disease and severe myelosuppression during azathioprine therapy. Gastroenterology. 2000; 118:1025–1030.
Article19. Takatsu N, Matsui T, Murakami Y, Ishihara H, Hisabe T, Nagahama T, et al. Adverse reactions to azathioprine cannot be predicted by thiopurine S-methyltransferase genotype in Japanese patients with inflammatory bowel disease. J Gastroenterol Hepatol. 2009; 24:1258–1264.
Article20. Ban H, Andoh A, Imaeda H, Kobori A, Bamba S, Tsujikawa T, et al. The multidrug-resistance protein 4 polymorphism is a new factor accounting for thiopurine sensitivity in Japanese patients with inflammatory bowel disease. J Gastroenterol. 2010; 45:1014–1021.
Article21. Uchiyama K, Nakamura M, Kubota T, Yamane T, Fujise K, Tajiri H. Thiopurine S-methyltransferase and inosine triphosphate pyrophosphohydrolase genes in Japanese patients with inflammatory bowel disease in whom adverse drug reactions were induced by azathioprine/6-mercaptopurine treatment. J Gastroenterol. 2009; 44:197–203.
Article22. Evans WE, Horner M, Chu YQ, Kalwinsky D, Roberts WM. Altered mercaptopurine metabolism, toxic effects, and dosage requirement in a thiopurine methyltransferase-deficient child with acute lymphocytic leukemia. J Pediatr. 1991; 119:985–989.
Article23. Kaskas BA, Louis E, Hindorf U, Schaeffeler E, Deflandre J, Graepler F, et al. Safe treatment of thiopurine S-methyltransferase deficient Crohn's disease patients with azathioprine. Gut. 2003; 52:140–142.
Article24. Grossman AB, Noble AJ, Mamula P, Baldassano RN. Increased dosing requirements for 6-mercaptopurine and azathioprine in inflammatory bowel disease patients six years and younger. Inflamm Bowel Dis. 2008; 14:750–755.
Article25. Nielsen OH, Vainer B, Rask-Madsen J. Review article: the treatment of inflammatory bowel disease with 6-mercaptopurine or azathioprine. Aliment Pharmacol Ther. 2001; 15:1699–1708.
Article26. Boonsrirat U, Angsuthum S, Vannaprasaht S, Kongpunvijit J, Hirankarn N, Tassaneeyakul W, et al. Azathioprine-induced fatal myelosuppression in systemic lupus erythematosus patient carrying TPMT*3C polymorphism. Lupus. 2008; 17:132–134.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Monitoring Thiopurine Metabolites in Korean Pediatric Patients with Inflammatory Bowel Disease
- Monitoring and Safety of Azathioprine Therapy in Inflammatory Bowel Disease
- Thiopurine S-methyltransferase Polymorphisms and the Relationship between the Mutant Alleles and the Adverse Effects in Systemic Lupus Erythematosus Patients Taking Azathioprine
- Genetic Polymorphism of Thiopurine Methyltransferase in Children with Acute Lymphoblastic Leukemia
- Rational Dosing of Azathioprine and 6-Mercaptopurine in Inflammatory Bowel Diseases