Clin Orthop Surg.
2014 Sep;6(3):312-317. 10.4055/cios.2014.6.3.312.
Biomechanical Analysis of Operative Methods in the Treatment of Extra-Articular Fracture of the Proximal Tibia
- Affiliations
-
- 1Department of Orthopedic Surgery, Kyungpook National University Hospital, Daegu, Korea. cwoh@knu.ac.kr
- 2Department of Orthopedic Surgery, Korea University Guro Hospital, Seoul, Korea.
- 3Solco Biomedical Institute, Pyeongtaek, Korea.
- KMID: 1794713
- DOI: http://doi.org/10.4055/cios.2014.6.3.312
Abstract
- BACKGROUND
To determine relative fixation strengths of a single lateral locking plate, a double construct of a locking plate, and a tibial nail used in treatment of proximal tibial extra-articular fractures.
METHODS
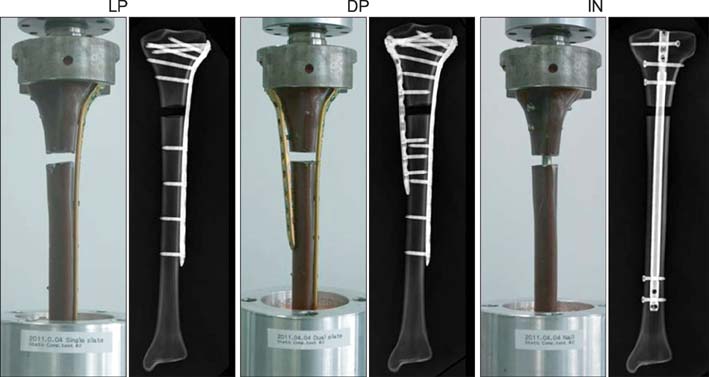
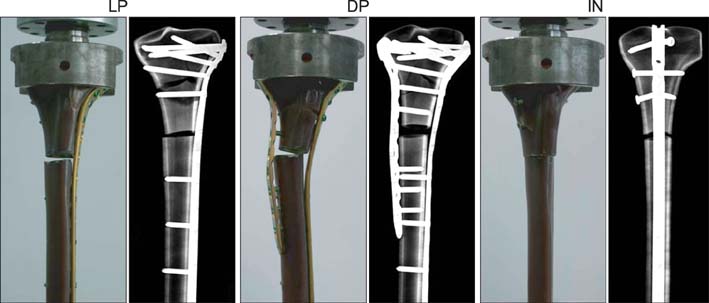
Three groups of composite tibial synthetic bones consisting of 5 specimens per group were included: lateral plating (LP) using a locking compression plate-proximal lateral tibia (LCP-PLT), double plating (DP) using a LCP-PLT and a locking compression plate-medial proximal tibia, and intramedullary nailing (IN) using an expert tibial nail. To simulate a comminuted fracture model, a gap osteotomy measuring 1 cm was created 8 cm below the knee joint. For each tibia, a minimal preload of 100 N was applied before loading to failure. A vertical load was applied at 25 mm/min until tibial failure.
RESULTS
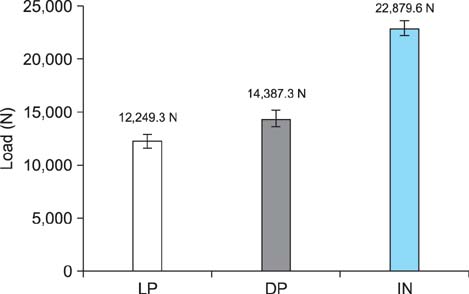
Under axial loading, fixation strength of DP (14,387.3 N; standard deviation [SD], 1,852.1) was 17.5% greater than that of LP (12,249.3 N; SD, 1,371.6), and 60% less than that of IN (22,879.6 N; SD, 1,578.8; p < 0.001, Kruskal-Wallis test). For ultimate displacement under axial loading, similar results were observed for LP (5.74 mm; SD, 1.01) and DP (4.45 mm; SD, 0.96), with a larger displacement for IN (5.84 mm; SD, 0.99). The median stiffness values were 2,308.7 N/mm (range, 2,147.5 to 2,521.4 N/mm; SD, 165.42) for the LP group, 4,128.2 N/mm (range, 3,028.1 to 4,831.0 N/mm; SD, 832.88) for the DP group, and 5,517.5 N/mm (range, 3,933.1 to 7,078.2 N/mm; SD, 1,296.19) for the IN group.
CONCLUSIONS
During biomechanical testing of a simulated comminuted proximal tibial fracture model, the DP proved to be stronger than the LP in terms of ultimate strength. IN proved to be the strongest; however, for minimally invasive osteosynthesis, which may be technically difficult to perform using a nail, the performance of the DP construct may lend credence to the additional use of a medial locking plate.
MeSH Terms
Figure
Reference
-
1. Phisitkul P, McKinley TO, Nepola JV, Marsh JL. Complications of locking plate fixation in complex proximal tibia injuries. J Orthop Trauma. 2007; 21(2):83–91.2. Hansen M, Blum J, Mehler D, Hessmann MH, Rommens PM. Double or triple interlocking when nailing proximal tibial fractures? A biomechanical investigation. Arch Orthop Trauma Surg. 2009; 129(12):1715–1719.3. Nork SE, Barei DP, Schildhauer TA, et al. Intramedullary nailing of proximal quarter tibial fractures. J Orthop Trauma. 2006; 20(8):523–528.4. Ricci WM, O'Boyle M, Borrelli J, Bellabarba C, Sanders R. Fractures of the proximal third of the tibial shaft treated with intramedullary nails and blocking screws. J Orthop Trauma. 2001; 15(4):264–270.5. Lindvall E, Sanders R, Dipasquale T, Herscovici D, Haidukewych G, Sagi C. Intramedullary nailing versus percutaneous locked plating of extra-articular proximal tibial fractures: comparison of 56 cases. J Orthop Trauma. 2009; 23(7):485–492.6. Gosling T, Schandelmaier P, Muller M, Hankemeier S, Wagner M, Krettek C. Single lateral locked screw plating of bicondylar tibial plateau fractures. Clin Orthop Relat Res. 2005; 439:207–214.7. Perren SM. Evolution of the internal fixation of long bone fractures. The scientific basis of biological internal fixation: choosing a new balance between stability and biology. J Bone Joint Surg Br. 2002; 84(8):1093–1110.8. Laflamme GY, Heimlich D, Stephen D, Kreder HJ, Whyne CM. Proximal tibial fracture stability with intramedullary nail fixation using oblique interlocking screws. J Orthop Trauma. 2003; 17(7):496–502.9. Krettek C, Miclau T, Schandelmaier P, Stephan C, Mohlmann U, Tscherne H. The mechanical effect of blocking screws ("Poller screws") in stabilizing tibia fractures with short proximal or distal fragments after insertion of small-diameter intramedullary nails. J Orthop Trauma. 1999; 13(8):550–553.10. Matthews DE, McGuire R, Freeland AE. Anterior unicortical buttress plating in conjunction with an unreamed interlocking intramedullary nail for treatment of very proximal tibial diaphyseal fractures. Orthopedics. 1997; 20(7):647–648.11. Boldin C, Fankhauser F, Hofer HP, Szyszkowitz R. Three-year results of proximal tibia fractures treated with the LISS. Clin Orthop Relat Res. 2006; 445:222–229.12. Cole PA, Zlowodzki M, Kregor PJ. Treatment of proximal tibia fractures using the less invasive stabilization system: surgical experience and early clinical results in 77 fractures. J Orthop Trauma. 2004; 18(8):528–535.13. Higgins TF, Klatt J, Bachus KN. Biomechanical analysis of bicondylar tibial plateau fixation: how does lateral locking plate fixation compare to dual plate fixation? J Orthop Trauma. 2007; 21(5):301–306.14. Mueller CA, Eingartner C, Schreitmueller E, et al. Primary stability of various forms of osteosynthesis in the treatment of fractures of the proximal tibia. J Bone Joint Surg Br. 2005; 87(3):426–432.15. Horwitz DS, Bachus KN, Craig MA, Peters CL. A biomechanical analysis of internal fixation of complex tibial plateau fractures. J Orthop Trauma. 1999; 13(8):545–549.16. Peindl RD, Zura RD, Vincent A, Coley ER, Bosse MJ, Sims SH. Unstable proximal extraarticular tibia fractures: a biomechanical evaluation of four methods of fixation. J Orthop Trauma. 2004; 18(8):540–545.17. Oh CW, Oh JK, Kyung HS, et al. Double plating of unstable proximal tibial fractures using minimally invasive percutaneous osteosynthesis technique. Acta Orthop. 2006; 77(3):524–530.18. Mueller KL, Karunakar MA, Frankenburg EP, Scott DS. Bicondylar tibial plateau fractures: a biomechanical study. Clin Orthop Relat Res. 2003; (412):189–195.19. D'Lima DD, Patil S, Steklov N, Slamin JE, Colwell CW Jr. Tibial forces measured in vivo after total knee arthroplasty. J Arthroplasty. 2006; 21(2):255–262.20. Zdero R, Rose S, Schemitsch EH, Papini M. Cortical screw pullout strength and effective shear stress in synthetic third generation composite femurs. J Biomech Eng. 2007; 129(2):289–293.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Extra-articulaf Fracture of Proximal Tibia
- Extra-articular Triplane Fracture of Distal Tibial Physis - Report of a Case
- Treatment of Extra-articular Proximal Tibial Fracture
- Comparison of Results Between Internal Fixation of Both Bones and Internal Fixation of the Only Tibia for Distal Tibial and Fibular Fractures
- The Proximal Tibial Metaphyseal Fracture (Extra-articular)