J Korean Med Sci.
2009 Feb;24(1):173-175. 10.3346/jkms.2009.24.1.173.
Tension Pneumothorax after Endoscopic Retrograde Pancreatocholangiogram
- Affiliations
-
- 1Department of Thoracic and Cardiovascular Surgery, Chonnam National University Hospital, Gwangju, Korea. hanse72@medigate.net
- KMID: 1794428
- DOI: http://doi.org/10.3346/jkms.2009.24.1.173
Abstract
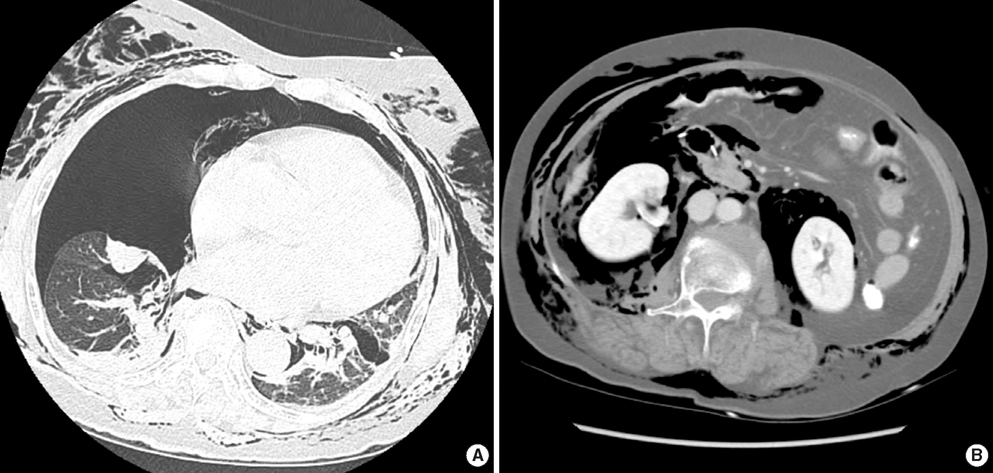
- We report a case of tension pneumothorax after an endoscopic sphincterotomy. A 78-yr-old woman presented with progressing dyspnea. She had undergone an endoscopic retrograde cholangiopancreatogram three days before due to acute cholecystitis. She underwent endoscopic sphincterotomy for stone extraction, but the procedure failed. On arrival to our hospital, she complained about severe dyspnea and she had subcutaneous emphysema. A computed tomogram scan revealed severe subcutaneous emphysema, right-side tension pneumothorax, and pneumoretroperitoneum. Contrast media injected through a transnasal biliary drainage catheter spilled from the second portion of the duodenum. A second abdominal computed tomogram showed multiple air densities in the retroperitoneum and peritoneal cavity, which were consistent with panperitonitis. We recommended an emergent laparotomic exploration, but the patient's guardians refused. She died eventually due to septic shock. Endoscopic retrograde cholangiopancreatogram is a popular procedure for biliary and pancreatic diseases, but it can cause severe complications such as intestinal perforation. Besides perforations, air can spread through the abdominal cavity, retroperitoneum, mediastinum, and the neck soft tissue, eventually causing pneumothorax. Early recognition and appropriate management is crucial to an optimal output of gastrointestinal perforation and pneumothorax.
MeSH Terms
Figure
Reference
-
1. Loperfido S, Angelini G, Benedetti G, Chilovi F, De Berardinis F, De Bernardin M, Ederle A, Fina P, Fratton A. Major early complications from diagnostic and therapeutic ERCP: a prospective multicenter study. Gastrointest Endosc. 1998. 48:1–10.
Article2. Pohle T, Domschke W, Lerch MM. Needle knife precut-induced bleeding from a "pancreatic cyst". Gastrointest Endosc. 2000. 52:564–566.
Article3. Stapfer M, Selby RR, Stain SC, Katkhouda N, Parekh D, Jabbour N, Garry D. Management of duodenal perforation after endoscopic retrograde cholangiopancreatography and sphincterotomy. Ann Surg. 2000. 232:191–198.
Article4. Zeno BR, Sahn SA. Colonoscopy-associated pneumothorax: a case of tension pneumothorax and review of the literature. Am J Med Sci. 2006. 332:153–155.
Article5. Morley AP, Lau JY, Young RJ. Tension pneumothorax complicating a perforation of a duodenal ulcer during ERCP with endoscopic sphincterotomy. Endoscopy. 1997. 29:332.
Article6. Gya D, Sali A, Angus D. Subcutaneous emphysema and pneumothorax following endoscopic sphincterotomy. Aust N Z J Surg. 1989. 59:900–902.
Article7. Maunder RJ, Pierson DJ, Hudson LD. Subcutaneous and mediastinal emphysema. Pathophysiology, diagnosis, and management. Arch Intern Med. 1984. 144:1447–1453.
Article8. Margantinis G, Sakorafas GH, Kostopoulos P, Kontou S, Tsiakos S, Arvanitidis D. Post-ERCP/endoscopic sphincterotomy duodenal perforation is not always a surgical emergency. Dig Liver Dis. 2006. 38:434–436.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Tension Pneumothorax Complicating Duodenal Microperforation after ERCP
- A rare complication: Tension pneumothorax after peroral endoscopic myotomy
- Tension pneumothorax after arthroscopic shoulder surgery: A case report
- Tension Pneumothorax Developed during General Anesthesia
- Tension Pneomothorax Related to General Anesthesia - 3 cases