Korean J Gastroenterol.
2014 Apr;63(4):239-243. 10.4166/kjg.2014.63.4.239.
Primary Aortoenteric Fistula to the Sigmoid Colon in Association with Intra-abdominal Abscess
- Affiliations
-
- 1Department of Internal Medicine, Kangwon National University College of Medicine, Chuncheon, Korea. drjaihwan@gmail.com
- KMID: 1791881
- DOI: http://doi.org/10.4166/kjg.2014.63.4.239
Abstract
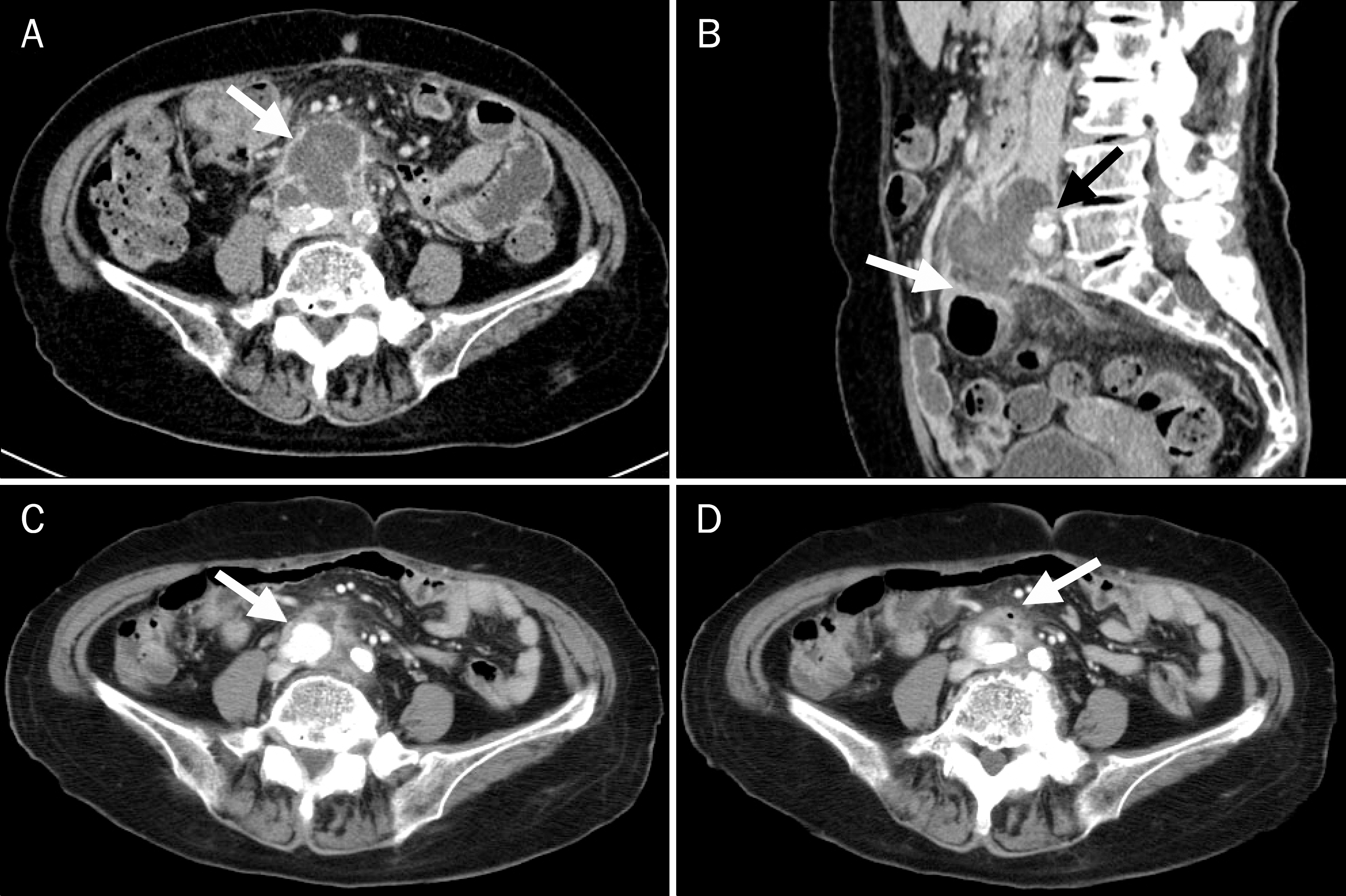
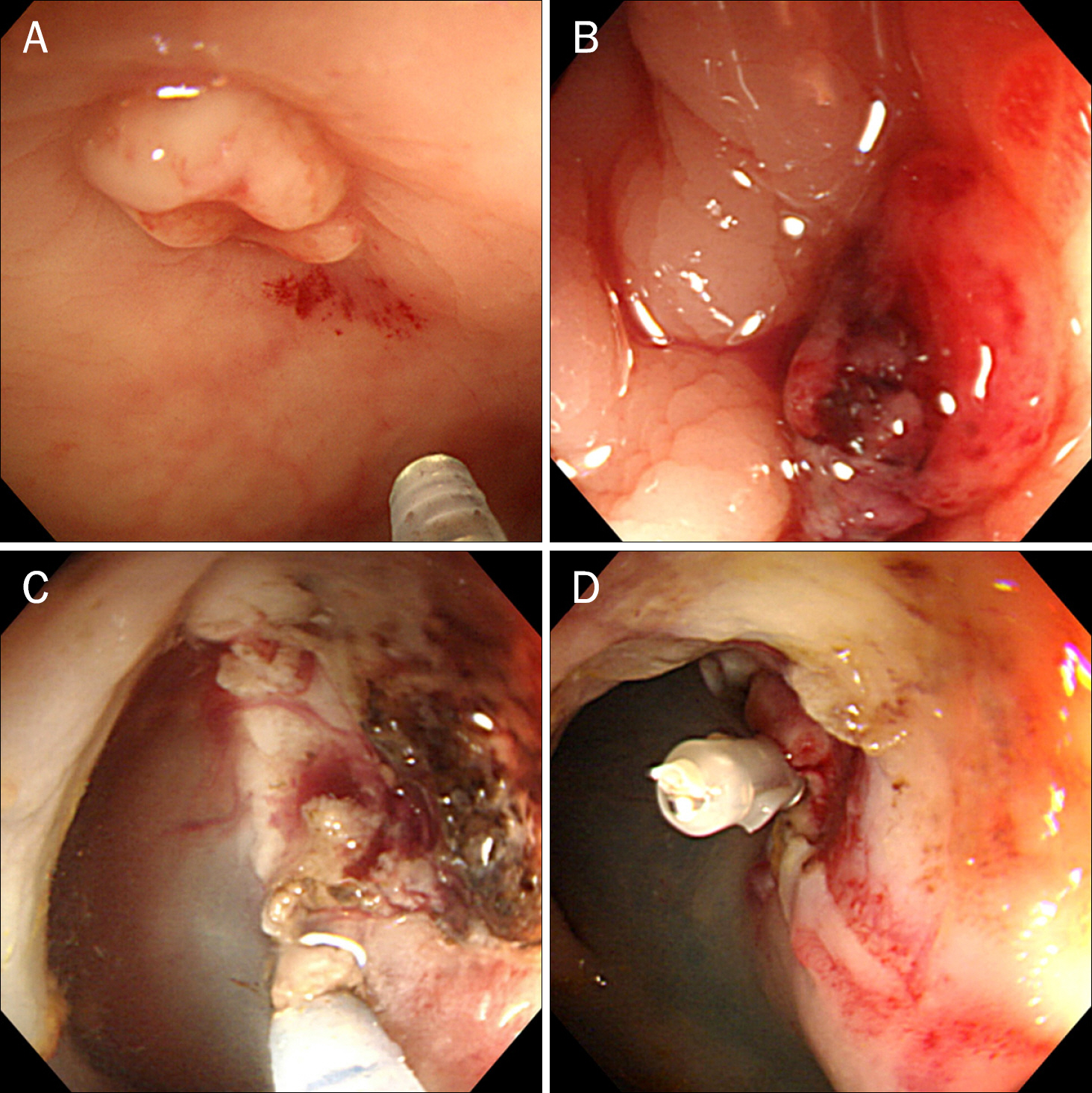
- Primary aortoenteric fistula (PAEF) is a rare but catastrophic cause of massive gastrointestinal bleeding. Diagnosis of PAEF is difficult to make and is frequently delayed without strong clinical suspicion. Timely surgical intervention is essential for patient's survival. We report on a case of an 86-year-old woman with no history of abdominal surgery, who presented with abdominal pain. Initially, computed tomography scan showed an intra-abdominal abscess, located anterior to the aortic bifurcation. However, she was discharged without treatment because of spontaneous improvement on a follow-up computed tomography scan, which showed a newly developed right common iliac artery aneurysm. One week later, she was readmitted due to recurrent abdominal pain. On the second day of admission, sudden onset of gastrointestinal bleeding occurred for the first time. After several endoscopic examinations, an aortoenteric fistula bleeding site was found in the sigmoid colon, and aortography showed progression of a right common iliac artery aneurysm. We finally concluded that intra-abdominal abscess induced an infected aortic aneurysm and enteric fistula to the sigmoid colon. This case demonstrated an extremely rare type of PAEF to the sigmoid colon caused by an infected abdominal aortic aneurysm, which has rarely been reported.
Keyword
MeSH Terms
-
Abdominal Abscess/*diagnosis/microbiology
Aged, 80 and over
Aorta, Abdominal/radiography
Aortic Aneurysm, Abdominal/*diagnosis/etiology
Bacteroides/isolation & purification
Bacteroides fragilis/isolation & purification
Colon, Sigmoid/radiography
Colonoscopy
Enterococcus/isolation & purification
Female
Fistula/*diagnosis
Humans
Tomography, X-Ray Computed
Figure
Reference
-
References
1. Voorhoeve R, Moll FL, de Letter JA, Bast TJ, Wester JP, Slee PH. Primary aortoenteric fistula: report of eight new cases and review of the literature. Ann Vasc Surg. 1996; 10:40–48.
Article2. Saers SJ, Scheltinga MR. Primary aortoenteric fistula. Br J Surg. 2005; 92:143–152.
Article3. Lemos DW, Raffetto JD, Moore TC, Menzoian JO. Primary aortoduodenal fistula: a case report and review of the literature. J Vasc Surg. 2003; 37:686–689.
Article4. Cooper A. The lectures of sir Astley Cooper on the principles and practice of surgery. 5th ed.Philadelphia: Haswell, Barrington and Haswell;1839.5. Sweeney MS, Gadacz TR. Primary aortoduodenal fistula: manifestation, diagnosis, and treatment. Surgery. 1984; 96:492–497.6. Steffes BC, O'Leary JP. Primary aortoduodenal fistula: a case report and review of the literature. Am Surg. 1980; 46:121–129.7. Perler BA, Ernst CB. Infected aneurysms. Veith FJ, Hobson RW, Williams RA, Wilson SE, editors. Vascular surgery: principles and practice. New York: McGraw-Hill;1994. p. 589–608.
Article8. Korkut AK, Arpinar E, Yasar T, Guney D. Primary aortoduodenal fistula complicated by abdominal aortic aneurysm. J Cardiovasc Surg (Torino). 2000; 41:113–115.9. Song Y, Liu Q, Shen H, Jia X, Zhang H, Qiao L. Diagnosis and management of primary aortoenteric fistulas–experience learned from eighteen patients. Surgery. 2008; 143:43–50.
Article10. Hill SL, Knott LH, Alexander RH. Recurrent aortoduodenal fistula: a lesson in management. Am Surg. 1982; 48:137–140.11. Lee JT, Saroyan RM, Belzberg G, Pianim NA, Bongard FS. Primary aortoenteric fistula: computed tomographic diagnosis of an atypical presentation. Ann Vasc Surg. 2001; 15:251–254.
Article12. Delgado J, Jotkowitz AB, Delgado B, Makarov V, Mizrahi S, Szendro G. Primary aortoduodenal fistula: Pitfalls and success in the endoscopic diagnosis. Eur J Intern Med. 2005; 16:363–365.
Article13. Jayarajan S, Napolitano LM, Rectenwald JE, Upchurch GR Jr. Primary aortoenteric fistula and endovascular repair. Vasc Endovascular Surg. 2009; 43:592–596.
Article14. Baril DT, Palchik E, Carroccio A, et al. Experience with endovascular abdominal aortic aneurysm repair in nonagenarians. J Endovasc Ther. 2006; 13:330–337.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Double Primary Aortoenteric Fistulae: A Case Report of Two Simultaneous Primary Aortoenteric Fistulae in One Patient
- Colouterine Fistula Caused by Diverticulitis of the Sigmoid Colon
- Colonic Diverticulitis Complicating Colo-ovarian Fistula and Tuboovarian Abscess Formation in on Old Woman
- Appendico-Sigmoid Fistula Due to Appendicitis
- Primary Aortoenteric Fistula of a Saccular Aneurysm: Case Study and Literature Review