J Korean Med Sci.
2014 Feb;29(2):281-286. 10.3346/jkms.2014.29.2.281.
Incidence and Risk Factors of Symptomatic Peripartum Diastasis of Pubic Symphysis
- Affiliations
-
- 1Department of Orthopedic Surgery, National University College of Medicine, Seoul, Korea.
- 2Department of Orthopedic Surgery, Chung-Ang University College of Medicine, Seoul, Korea. hayongch@naver.com
- 3Department of Obstetrics and Gynecology, Seoul National University College of Medicine, Seoul, Korea.
- 4Department of Orthopedic Surgery, Gyeongsang National University School of Medicine, Jinju, Korea.
- KMID: 1789989
- DOI: http://doi.org/10.3346/jkms.2014.29.2.281
Abstract
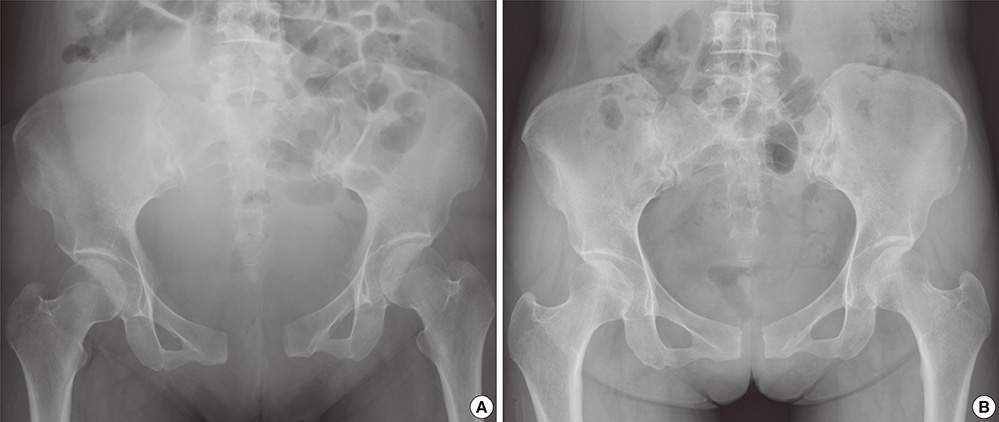
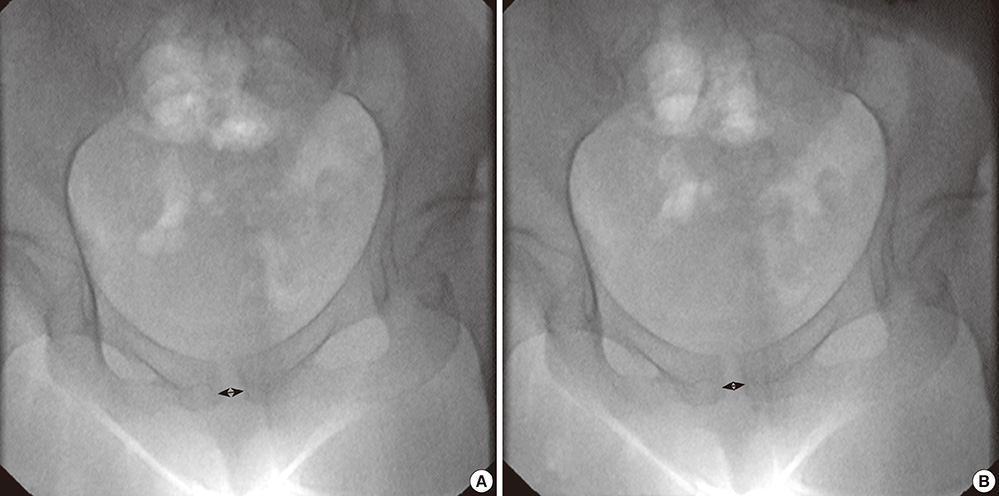
- This study was undertaken to determine incidence, associated risk factors, and clinical outcomes of a diastasis of pubic symphysis. Among 4,151 women, who delivered 4,554 babies at the Department of Obstetrics of Seoul National University Bundang hospital from January 2004 to December 2006, eleven women were diagnosed as having a symptomatic diastasis of pubic symphysis. We estimated the incidence of the diastasis and identified the associated risk factors. To evaluate the pain relief and reduction of diastasis we followed up the 11 diastatic patients. The incidence of the diastasis was 1/385. Primiparity (P = 0.010) and twin gestation (P = 0.016) appeared as risk factors for diastasis by univairable analysis; and twin gestation appeared to be the only risk factor (P = 0.006) by logistic analysis. Two patients were operated due to intractable pain; and the remaining nine patients were treated conservatively. The diastatic gap decreased to less than 1.5 cm by 2 to 6 weeks after the diagnosis and then remained stationary. At a mean follow-up of 22.1 months (range, 12 to 47 months), five of 11 patients had persistent symphysis pubis dysfunction. Diastasis is more frequent than generally acknowledged. Pregnant women with multiple gestations should be informed about the potential risk of pubic symphysis diastasis.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Outcome of Internal Fixation and Corticocancellous Grafting of Symphysis Pubis Diastasis Which Developed after Malunion of Pubic Rami Fracture
Hasan Bombaci
Hip Pelvis. 2017;29(2):150-153. doi: 10.5371/hp.2017.29.2.150.
Reference
-
1. Crim MW, Moss SW. Pelvic diastasis in pregnancy. Am Fam Physician. 1987; 35:185–186.2. Callahan JT. Separation of the symphysis pubis. Am J Obstet Gynecol. 1953; 66:281–293.3. Moon WN, Han JY, Oh HJ, Suh SW. Diastasis of the symphysis pubis after delivery. J Korean Orthop Assoc. 2001; 36:473–478.4. Cibils LA. Rupture of the symphysis pubis: a case report. Obstet Gynecol. 1971; 38:407–410.5. Braddon SA. Relaxin-dependent adenosine 6',5'-monophosphate concentration changes in the mouse pubic symphysis. Endocrinology. 1978; 102:1292–1299.6. Culligan P, Hill S, Heit M. Rupture of the symphysis pubis during vaginal delivery followed by two subsequent uneventful pregnancies. Obstet Gynecol. 2002; 100:1114–1117.7. Dhar S, Anderton JM. Rupture of the symphysis pubis during labor. Clin Orthop Relat Res. 1992; (283):252–257.8. Ku SJ, Kim SB, Kim JH, Park HY, Kim HJ. Clinical analysis of the perinatal pubic bone separation. Korean J Obstet Gynecol. 2006; 49:315–321.9. Cowling PD, Rangan A. A case of postpartum pubic symphysis diastasis. Injury. 2010; 41:657–659.10. Chang JL, Wu V. External fixation of pubic symphysis diastasis from postpartum trauma. Orthopedics. 2008; 31:493.11. Chang D, Markman BS. Images in clinical medicine: spontaneous resolution of a pubic-symphysis diastasis. N Engl J Med. 2002; 346:39.12. Reis RA, Baer JL, Arens RA, Stewart E. Traumatic separation of the symphysis pubis during spontaneous labor. Surg Gynecol Obstet. 1932; 55:336–354.13. Taylor RN, Sonson RD. Separation of the pubic symphysis: an underrecognized peripartum complication. J Reprod Med. 1986; 31:203–206.14. Heath T, Gherman RB. Symphyseal separation, sacroiliac joint dislocation and transient lateral femoral cutaneous neuropathy associated with McRoberts' maneuver: a case report. J Reprod Med. 1999; 44:902–904.15. Moon WN, Han JY. Radiographic appearance of the symphysis pubis: criteria of diastasis of symphysis pubis after normal delivery. J Korean Orthop Assoc. 1999; 34:969–972.16. Hagen R. Pelvic girdle relaxation from an orthopaedic point of view. Acta Orthop Scand. 1974; 45:550–563.17. Kharrazi FD, Rodgers WB, Kennedy JG, Lhowe DW. Parturition-induced pelvic dislocation: a report of four cases. J Orthop Trauma. 1997; 11:277–281.18. Leadbetter RE, Mawer D, Lindow SW. Symphysis pubis dysfunction: a review of the literature. J Matern Fetal Neonatal Med. 2004; 16:349–354.19. So YH, Park SG, Kal CW, Kim MJ, Lee JH, Kim YC. Separation of symphysis pubis during vaginal delivery - report of 5 cases. Korean J Obstet Gynecol. 2000; 43:2310–2314.20. Seth S, Das B, Salhan S. A severe case of pubic symphysis diastasis in pregnancy. Eur J Obstet Gynecol Reprod Biol. 2003; 106:230–232.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Outcome of Internal Fixation and Corticocancellous Grafting of Symphysis Pubis Diastasis Which Developed after Malunion of Pubic Rami Fracture
- Diastasis of the Symphysis Pubis During Vaginal Delivery
- A case of disruption of symphysis pubis diagnosed after delivery of a primigravida
- Unusual Dislocation of the Symphysis Pubis: A Case Report
- Risk factors for lower urinary tract injuries in patients with traumatic pelvic fractures