Yonsei Med J.
2007 Dec;48(6):988-993. 10.3349/ymj.2007.48.6.988.
Spinal Cord Tumors of the Thoracolumbar Junction Requiring Surgery: A Retrospective Review of Clinical Features and Surgical Outcome
- Affiliations
-
- 1Department of Neurosurgery, Yonsei University College of Medicine, Seoul, Korea. ydoheum@yuhs.ac
- KMID: 1786214
- DOI: http://doi.org/10.3349/ymj.2007.48.6.988
Abstract
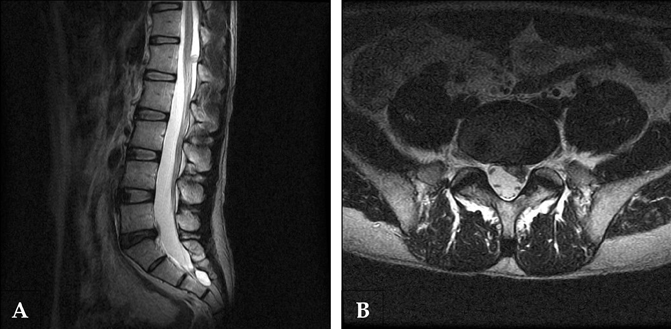
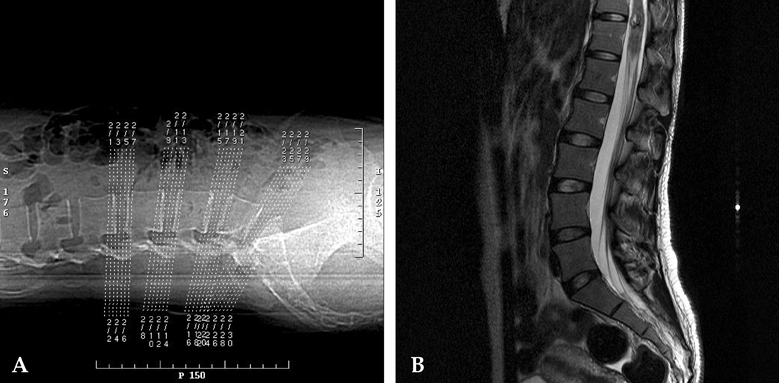
- PURPOSE: A retrospective review of medical records and imaging studies. To investigate characteristic clinical features and surgical outcomes of spinal cord tumors (SCTs) of the thoracolumbar junction (TLJ). The spinal cord transitions to the cauda equina in the TLJ. The TLJ contains the upper and lower motor neurons of the spinal cord and cauda equina. As a result, the clinical features of lesions in the TLJ vary, and these anatomical characteristics may affect surgical outcome. MATERIALS AND METHODS: Pathological diagnosis, clinical features, neurological signs, and surgical outcomes were investigated in 76 patients surgically treated at our institute for SCTs arising from T11 to L2. The patients were divided into epiconus (T11-12, n=18) and conus groups (L1-2, n=58). RESULTS: Patients in the epiconus group had hyperactive deep tendon reflexes (DTRs), while those in the conus group had hypoactive DTRs (p < 0.05). Nine patients were misdiagnosed with intervertebral disc diseases (IVDs) before correct diagnoses were made. It was impossible to definitively determine the exact cause of symptoms in four patients who had both SCTs and IVDs. CONCLUSION: Among SCTs of the TLJ, the epiconus group displayed upper motor neuron syndrome and the conus group displayed lower motor neuron syndrome. SCTs of the TLJ were frequently misdiagnosed as IVDs due to symptomatic similarities. SCTs of the TLJ should be included in differential diagnosis of back and leg pain, and it is highly recommended that routine lumbar magnetic resonance imaging include the TLJ.
MeSH Terms
Figure
Reference
-
1. Tokuhashi Y, Matsuzaki H, Uematsu Y, Oda H. Symptoms of thoracolumbar junction disc herniation. Spine. 200. 26:E512–E518.
Article2. Lyu RK, Chang HS, Tang LM, Chen ST. Thoracic disc herniation mimicking acute lumbar disc disease. Spine. 1999. 24:416–418.
Article3. Traul DE, Shaffrey ME, Schiff D. Part I: spinal-cord neoplasms-intradural neoplasms. Lancet Oncol. 2007. 8:35–45.
Article4. Harzallah L, Bouajina E, Ghannouchi M, Amara H, Ben Chérifa L, Kraiem CH. Low back pain and sciatica as the presenting symptoms of neurinoma near the conus medullaris. Contribution of magnetic resonance imaging. Joint Bone Spine. 2005. 72:187–189.
Article5. Amezyane T, Pouit B, Bassou D, Lecoules S, Desramé J, Blade JS, et al. A rare cause of sciatica. Rev Med Interne. 2006. 27:494–496.6. Komatsu Y, Narushima K, Kobayashi E, Ebihara R, Nose T, Maki Y. Small cauda equina neurinoma detected by MR imaging. AJNR Am J Neuroradiol. 1988. 9:1243.7. Shimada Y, Miyakoshi N, Kasukawa Y, Hongo M, Ando S, Itoi E. Clinical features of cauda equina tumors requiring surgical treatment. Tohoku J Exp Med. 2006. 209:1–6.
Article8. Sloof JL, Kernohan JW, MacCarthy CS. Primary Intramedullary Tumors of the Spinal Cord and Filum Terminale. 1964. Philadelphia, PA: WB Saunders.9. Cooper PR. Outcome after operative treatment of intramedullary spinal cord tumors in adults: intermediate and long-term results in 51 patients. Neurosurgery. 1989. 25:855–859.
Article10. Mathew P, Todd NV. Intradural conus and cauda equina tumours: a retrospective review of presentation, diagnosis and early outcome. J Neurol Neurosurg Psychiatry. 1993. 56:69–74.
Article11. Fearnside MR, Adams CB. Tumours of the cauda equina. J Neurol Neurosurg Psychiatry. 1978. 41:24–31.
Article12. Groen RJ, Kuster JA, Noske DP, Tjahja SI, de Vries L. Nocturnal back pain; a misdiagnosed symptom of spinal tumor. Ned Tijdschr Geneeskd. 2001. 145:2134–2138.13. Bauer M, Brock M, Cervós-Navarro J, Prosenc N, Marx P. [Intraspinal neurinoma in the thoracolumbar junction presenting unusual symptoms. The differential diagnosis of lumbago]. Dtsch Med Wochenschr. 1994. 119:628–630.
Article14. Jo BJ, Lee SH, Chung SE, Paeng SS, Kim HS, Yoon SW, et al. Pure epidural cavernous hemangioma of the cervical spine that presented with an acute sensory deficit caused by hemorrhage. Yonsei Med J. 2006. 47:877–880.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Surgical Planning for Thoracolumar Spine Fracture
- Huge Thoracolumbar Extradural Arachnoid Cyst
- Spinal Cord Tumors: An Analysis of 654 Cases(1973-1999)
- Pain Around the Posterior Iliac Crest of Thoracolumbar Origin
- Long Term Outcome of Non-Dysraphic Intramedullary Spinal Cord Lipomas in Adults: Case Series and Review