J Korean Med Sci.
2014 May;29(5):739-742. 10.3346/jkms.2014.29.5.739.
Gastroplasty for Esophageal Perforation after Endoscopic Balloon Dilatation for Achalasia: Two Cases
- Affiliations
-
- 1Department of Cardiothoracic Surgery, Soonchunhyang University Hospital, Seoul, Korea. stingkhz@schmc.ac.kr
- KMID: 1786119
- DOI: http://doi.org/10.3346/jkms.2014.29.5.739
Abstract
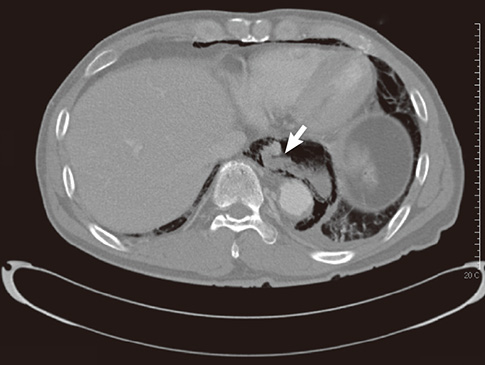
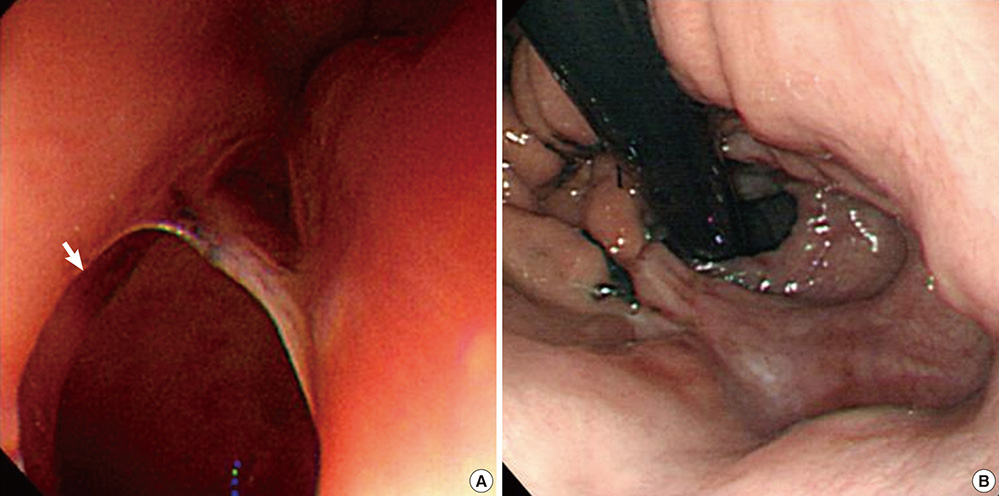
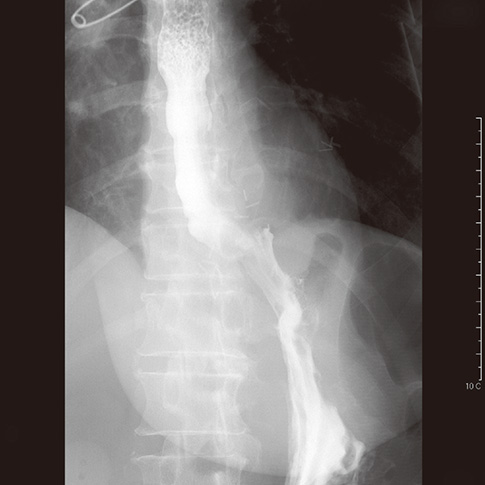
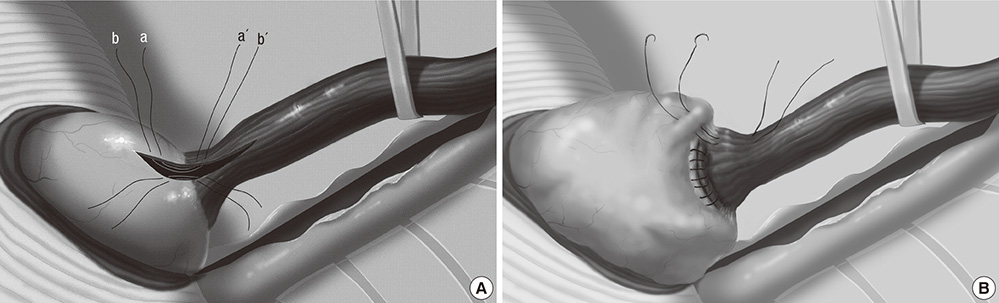
- Esophageal perforation after endoscopic forceful pneumatic dilatation for achalasia is a devastating complication and surgical treatment is necessary. A 65-yr-old man and a 54-yr-old woman referred for esophageal perforation two hours after pneumatic dilatation and during the procedure, respectively. Gastroplasties through thoracotomy were performed in both cases and their recoveries were uneventful. The esophagogram with gastrografin on the post-operative 8th day did not show any passage disturbance or leakage at the anastomosis site. On the follow-up endoscopy 4 to 6 months after operation revealed that reflux esophagitis of LA classification A were noted in the both patients. They did not complain any reflux symptom or dysphagia for 9 to 13 months after operation. Instead of the most widely used procedure; primary repair of perforation site, wrapping with intercostal muscle flap and esophagomyotomy, gastroplasty was performed in two cases of iatrogenic esophageal perforation in achalasia and experienced good results.
MeSH Terms
Figure
Reference
-
1. Hunt DR, Wills VL, Weis B, Jorgensen JO, DeCarle DJ, Coo IJ. Management of esophageal perforation after pneumatic dilation for achalasia. J Gastrointest Surg. 2000; 4:411–415.2. Vanuytsel T, Lerut T, Coosemans W, Vanbeckevoort D, Blondeau K, Boeckxstaens G, Tack J. Conservative management of esophageal perforations during pneumatic dilation for idiopathic esophageal achalasia. Clin Gastroenterol Hepatol. 2012; 10:142–149.3. Park H, Keum DY, Park NH, Park CK, Lee KS. Clinical analysis and treatment of esophageal perforation. Korean J Thorac Cardiovasc Surg. 2006; 39:111–116.4. Brinster CJ, Singhal S, Lee L, Marshall MB, Kaiser LR, Kucharczuk JC. Evolving options in the management of esophageal perforation. Ann Thorac Surg. 2004; 77:1475–1483.5. Urbani M, Mathisen DJ. Repair of esophageal perforation after treatment for achalasia. Ann Thorac Surg. 2000; 69:1609–1611.6. Richardson JD. Management of esophageal perforations: the value of aggressive surgical treatment. Am J Surg. 2005; 190:161–165.7. Chen LQ, Chughtai T, Sideris L, Nastos D, Taillefer R, Ferraro P, Duranceau A. Long-term effects of myotomy and partial fundoplication for esophageal achalasia. Dis Esophagus. 2002; 15:171–179.8. Migliore M, Arcerito M, Vagliasindi A, Puleo R, Basile F, Deodato G. The place of Belsey Mark IV fundoplication in the era of laparoscopic surgery. Eur J Cardiothorac Surg. 2003; 24:625–630.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Balloon Catheter Dilatation in Esophageal Achalasia: Long Term Follow-Up
- Non-surgical treatment of esophageal perforation after pneumatic balloon dilatation for primary achalasia
- Endoscopic Treatment of Primary Esophageal Motility Disorders
- Two Cases of Achalasia with Normal Lower Esophageal Sphincter Pressure
- Thoracoscopic Surgery for Esophageal Perforation and Achalasia: Two cases report