J Korean Med Sci.
2011 Jun;26(6):832-835. 10.3346/jkms.2011.26.6.832.
Synchronous Ectopic Pancreatoblastoma in a Child: A Case Report
- Affiliations
-
- 1Department of Radiology, the First Affiliated Hospital of ZhengZhou University, Zhengzhou, Henan, China. yangzhihao1365380@126.com
- KMID: 1785973
- DOI: http://doi.org/10.3346/jkms.2011.26.6.832
Abstract
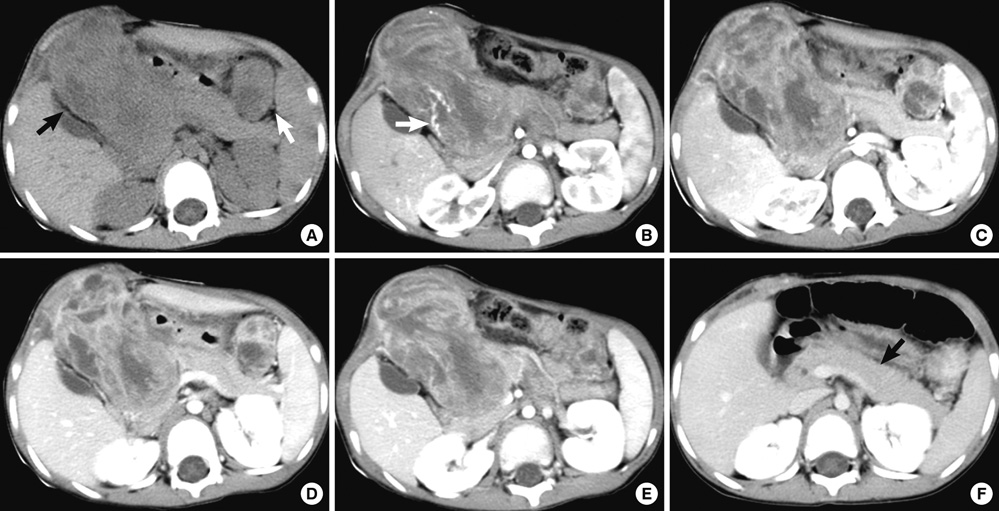
- Pancreatoblastoma is a rare primary pancreatic neoplasm of children that may arise in any portion of the pancreas. We report a case of a 3-yr-old boy who presented to with abdominal pain our hospital and a progressive bulge in his right abdomen. Biochemical evaluation and serum levels of tumoral markers were within reference limits. On the computed tomography, two tumors were found. One located in the head of the pancreas; however, a laparotomy revealed that the head of pancreas was compressed but normal. The other was in the left abdomen near the spleen and the tail of the pancreas. The diagnosis of two synchronous pancreatoblastoma originating from the omentum was confirmed by pathology. Therefore, a pancreatoblastoma should be considered when a large well-defined, lobulated, and heterogeneous mass is identified in the pancreas of children. In addition, an ectopic pancreatoblastoma should be considered when identified within or near the ectopic pancreatic tissue.
Keyword
MeSH Terms
Figure
Reference
-
1. Becker WF. Pancreatoduodenectomy for carcinoma of the pancreas in an infant; report of a case. Ann Surg. 1957. 145:864–872.2. Cavallini A, Falconi M, Bortesi L, Crippa S, Barugola G, Butturini G. Pancreatoblastoma in adults: a review of the literature. Pancreatology. 2009. 9:73–80.3. Chung EM, Travis MD, Conran RM. Pancreatic tumors in children: radiologic-pathologic correlation. Radiographics. 2006. 26:1211–1238.4. Saif MW. Pancreatoblastoma. JOP. 2007. 8:55–63.5. Yang X, Wang X. Imaging findings of pancreatoblastoma in 4 children including a case of ectopic pancreatoblastoma. Pediatr Radiol. 2010. 40:1609–1614.6. Ogata H, Oshio T, Ishibashi H, Takano S, Yagi M. Heterotopic pancreas in children: review of the literature and report of 12 cases. Pediatr Surg Int. 2008. 24:271–275.7. Makhlouf HR, Almeida JL, Sobin LH. Carcinoma in jejunal pancreatic heterotopia. Arch Pathol Lab Med. 1999. 123:707–711.8. Cho JS, Shin KS, Kwon ST, Kim JW, Song CJ, Noh SM, Kang DY, Kim HY, Kang HK. Heterotopic pancreas in the stomach: CT findings. Radiology. 2000. 217:139–144.9. Shin SS, Jeong YY, Kang HK. Giant heterotopic pancreas in the jejunal mesentery. AJR Am J Roentgenol. 2007. 189:W262–W263.10. Rubesin SE, Furth EE, Birnbaum BA, Rowling SE, Herlinger H. Ectopic pancreatitis complicated by pancreatitis and pseudocyst formation mimicking jejunal diverticulitis. Br J Radiol. 1997. 70:311–313.11. Emerson L, Layfield LJ, Rohr LR, Dayton MT. Adenocarcinoma arising in association with gastric heterotopic pancreas: a case report and review of the literature. J Surg Oncol. 2004. 87:53–57.12. Guillou L, Nordback P, Gerber C, Schneider RP. Ductal adenocarcinoma arising in a heterotopic pancreas situated in a hiatal hernia. Arch Pathol Lab Med. 1994. 118:568–571.13. Roebuck DJ, Yuen MK, Wong YC, Shing MK, Lee CW, Li CK. Imaging features of pancreatoblastoma. Pediatr Radiol. 2001. 31:501–506.14. Montemarano H, Lonergan GJ, Bulas DI, Selby DM. Pancreatoblastoma: imaging findings in 10 patients and review of the literature. Radiology. 2000. 214:476–482.15. Gupta AK, Mitra DK, Berry M, Dinda AK, Bhatnagar V. Sonography and CT of pancreatoblastoma in children. AJR Am J Roentgenol. 2000. 174:1639–1641.16. Levey JM, Banner BF. Adult pancreatoblastoma: a case report and review of the literature. Am J Gastroenterol. 1996. 91:1841–1844.17. Chun Y, Kim W, Park K, Lee S, Jung S. Pancreatoblastoma. J Pediatr Surg. 1997. 32:1612–1615.18. Ogawa B, Okinaga K, Obana K, Nakamura K, Hattori T, Ito T, Yanagawa Y, Tanaka F, Imamura T. Pancreatoblastoma treated by delayed operation after effective chemotherapy. J Pediatr Surg. 2000. 35:1663–1665.