Clin Orthop Surg.
2014 Jun;6(2):230-235. 10.4055/cios.2014.6.2.230.
Plain Radiologic Findings and Chronological Changes of Incipient Phase Osteosarcoma Overlooked by Primary Physicians
- Affiliations
-
- 1Department of Orthopedic Surgery, Korea Cancer Center Hospital, Seoul, Korea. dgjeon@kcch.re.kr
- KMID: 1784672
- DOI: http://doi.org/10.4055/cios.2014.6.2.230
Abstract
- BACKGROUND
We assessed the plain radiographic characteristics of 10 cases of osteosarcomas during the initial painful period that had been overlooked by a primary physician. In addition, we evaluated chronologic changes in radiographic findings from initial symptomatic period to the time of accurate diagnosis.
METHODS
The clinical records were reviewed for clinical parameters including age, sex, location, presenting symptoms, initial diagnosis, duration from initial symptoms to definite diagnosis, and initial and follow-up plain radiographic findings of the lesion.
RESULTS
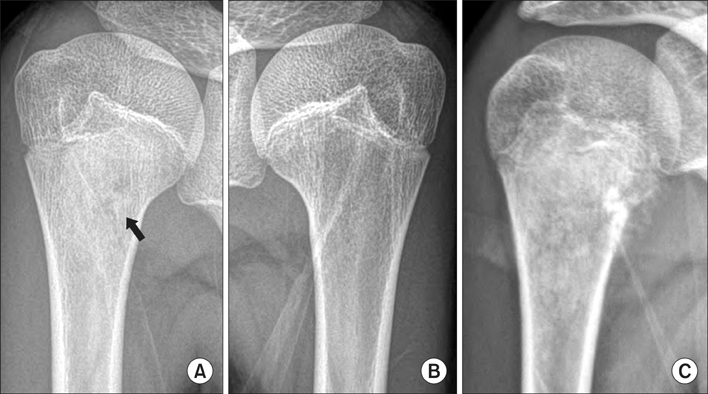
Initial clinical diagnoses included a sprain in 6, growing pain in 2, stress fracture in 1, and infection in 1 patient. Initial plain radiographic findings were trabecular destruction (100%), cortical disruption (60%), periosteal reaction (60%), and soft tissue mass (10%). Intramedullary matrix changes were osteosclerosis in 6 and osteolysis in 4 patients. On progression, 4 cases with minimal sclerosis changed to osteoblastic lesion in 3 patients and osteolytic lesion in 1. Four cases with faint osteolytic foci transformed into osteolytic lesion in 3 and mixed pattern in 1.
CONCLUSIONS
Notable plain radiologic findings of incipient-stage osteosarcoma include trabecular disruption along with faint osteosclerosis or osteolysis. In symptomatic patients with trabecular destruction, additional imaging study including magnetic resonance imaging should be performed to exclude osteosarcoma in the incipient phase, even without radiologic findings suggesting malignant tumor, such as cortical destruction or periosteal reaction.
MeSH Terms
Figure
Reference
-
1. Sneppen O, Hansen LM. Presenting symptoms and treatment delay in osteosarcoma and Ewing's sarcoma. Acta Radiol Oncol. 1984; 23(2-3):159–162.2. Widhe B, Widhe T. Initial symptoms and clinical features in osteosarcoma and Ewing sarcoma. J Bone Joint Surg Am. 2000; 82(5):667–674.3. Kim MS, Cho WH, Song WS, Lee SY, Jeon DG. time dependency of prognostic factors in patients with stage II osteosarcomas. Clin Orthop Relat Res. 2007; 463:157–165.4. Jeon DG, Lee SY, Cho WH, Song WS, Park JH. Primary osteosarcoma in patients older than 40 years of age. J Korean Med Sci. 2006; 21(4):715–718.5. de Santos LA, Edeiken BS. Subtle early osteosarcoma. Skeletal Radiol. 1985; 13(1):44–48.6. Andresen KJ, Sundaram M, Unni KK, Sim FH. Imaging features of low-grade central osteosarcoma of the long bones and pelvis. Skeletal Radiol. 2004; 33(7):373–379.7. Bertoni F, Unni KK, McLeod RA, Dahlin DC. Osteosarcoma resembling osteoblastoma. Cancer. 1985; 55(2):416–426.8. Tsuneyoshi M, Dorfman HD. Epiphyseal osteosarcoma: distinguishing features from clear cell chondrosarcoma, chondroblastoma, and epiphyseal enchondroma. Hum Pathol. 1987; 18(6):644–651.9. Rosenberg ZS, Lev S, Schmahmann S, Steiner GC, Beltran J, Present D. Osteosarcoma: subtle, rare, and misleading plain film features. AJR Am J Roentgenol. 1995; 165(5):1209–1214.10. Kim MS, Lee SY, Cho WH, et al. Prognostic effects of doctor-associated diagnostic delays in osteosarcoma. Arch Orthop Trauma Surg. 2009; 129(10):1421–1425.11. Jeon DG, Lee SY, Kim JW. Bone primary sarcomas undergone unplanned intralesional procedures - the possibility of limb salvage and their oncologic results. J Surg Oncol. 2006; 94(7):592–598.12. Kim MS, Lee SY, Cho WH, et al. Relationships between plain-film radiographic patterns and clinicopathologic variables in AJCC stage II osteosarcoma. Skeletal Radiol. 2008; 37(11):997–1001.13. Ayerza MA, Muscolo DL, Aponte-Tinao LA, Farfalli G. Effect of erroneous surgical procedures on recurrence and survival rates for patients with osteosarcoma. Clin Orthop Relat Res. 2006; 452:231–235.