Clin Orthop Surg.
2014 Jun;6(2):138-145. 10.4055/cios.2014.6.2.138.
Treatment Results of a Periprosthetic Femoral Fracture Case Series: Treatment Method for Vancouver Type B2 Fractures Can Be Customized
- Affiliations
-
- 1Department of Orthopaedic Surgery, Kobe University Graduate School of Medicine, Kobe, Japan. tniikura@med.kobe-u.ac.jp
- KMID: 1784658
- DOI: http://doi.org/10.4055/cios.2014.6.2.138
Abstract
- BACKGROUND
Currently, an algorithmic approach for deciding treatment options according to the Vancouver classification is widely used for treatment of periprosthetic femoral fractures after hip arthroplasty. However, this treatment algorithm based on the Vancouver classification lacks consideration of patient physiology and surgeon's experience (judgment), which are also important for deciding treatment options. The purpose of this study was to assess the treatment results and discuss the treatment options using a case series.
METHODS
Eighteen consecutive cases with periprosthetic femoral fractures after total hip arthroplasty and hemiarthroplasty were retrospectively reviewed. A locking compression plate system was used for osteosynthesis during the study period. The fracture type was determined by the Vancouver classification. The treatment algorithm based on the Vancouver classification was generally applied, but was modified in some cases according to the surgeon's judgment. The reasons for modification of the treatment algorithm were investigated. Mobility status, ambulatory status, and social status were assessed before the fracture and at the latest follow-up. Radiological results including bony union and stem stability were also evaluated.
RESULTS
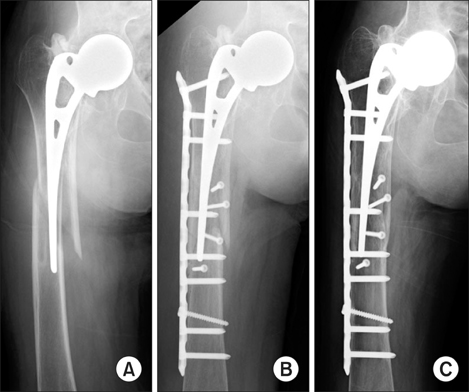
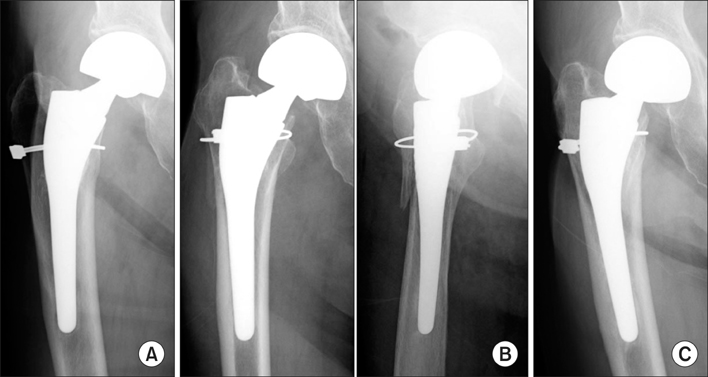
Thirteen cases were treated by osteosynthesis, two by revision arthroplasty and three by conservative treatment. Four cases of type B2 fractures with a loose stem, in which revision arthroplasty is recommended according to the Vancouver classification, were treated by other options. Of these, three were treated by osteosynthesis and one was treated conservatively. The reasons why the three cases were treated by osteosynthesis were technical difficulty associated with performance of revision arthroplasty owing to severe central migration of an Austin-Moore implant in one case and subsequent severe hip contracture and low activity in two cases. The reasons for the conservative treatment in the remaining case were low activity, low-grade pain, previous wiring around the fracture and light weight. All patients obtained primary bony union and almost fully regained their prior activities.
CONCLUSIONS
We suggest reaching a decision regarding treatment methods of periprosthetic femoral fractures by following the algorithmic approach of the Vancouver classification in addition to the assessment of each patient's hip joint pathology, physical status and activity, especially for type B2 fractures. The customized treatments demonstrated favorable overall results.
MeSH Terms
Figure
Cited by 1 articles
-
Could Patient Undergwent Surgical Treatment for Periprosthetic Femoral Fracture after Hip Arthroplasty Return to Their Status before Trauma?
Long Zheng, Woo-Yong Lee, Deuk-Soo Hwang, Chan Kang, Chang-Kyun Noh
Hip Pelvis. 2016;28(2):90-97. doi: 10.5371/hp.2016.28.2.90.
Reference
-
1. Berry DJ. Epidemiology: hip and knee. Orthop Clin North Am. 1999; 30(2):183–190.2. Haddad FS, Duncan CP, Berry DJ, Lewallen DG, Gross AE, Chandler HP. Periprosthetic femoral fractures around well-fixed implants: use of cortical onlay allografts with or without a plate. J Bone Joint Surg Am. 2002; 84(6):945–950.3. Ricci WM, Bolhofner BR, Loftus T, Cox C, Mitchell S, Borrelli J Jr. Indirect reduction and plate fixation, without grafting, for periprosthetic femoral shaft fractures about a stable intramedullary implant. J Bone Joint Surg Am. 2005; 87(10):2240–2245.4. Tsiridis E, Narvani AA, Timperley JA, Gie GA. Dynamic compression plates for Vancouver type B periprosthetic femoral fractures: a 3-year follow-up of 18 cases. Acta Orthop. 2005; 76(4):531–537.5. Macdonald SJ, Paprosky WG, Jablonsky WS, Magnus RG. Periprosthetic femoral fractures treated with a long-stem cementless component. J Arthroplasty. 2001; 16(3):379–383.6. Park MS, Lee YK, Yang KH, Shin SJ. Management of periprosthetic femoral fractures. J Arthroplasty. 2003; 18(7):903–906.7. Lee SR, Bostrom MP. Periprosthetic fractures of the femur after total hip arthroplasty. Instr Course Lect. 2004; 53:111–118.8. Kaab MJ, Stockle U, Schutz M, Stefansky J, Perka C, Haas NP. Stabilisation of periprosthetic fractures with angular stable internal fixation: a report of 13 cases. Arch Orthop Trauma Surg. 2006; 126(2):105–110.9. O'Toole RV, Gobezie R, Hwang R, et al. Low complication rate of LISS for femur fractures adjacent to stable hip or knee arthroplasty. Clin Orthop Relat Res. 2006; 450:203–210.10. Chakravarthy J, Bansal R, Cooper J. Locking plate osteosynthesis for Vancouver Type B1 and Type C periprosthetic fractures of femur: a report on 12 patients. Injury. 2007; 38(6):725–733.11. Erhardt JB, Grob K, Roderer G, Hoffmann A, Forster TN, Kuster MS. Treatment of periprosthetic femur fractures with the non-contact bridging plate: a new angular stable implant. Arch Orthop Trauma Surg. 2008; 128(4):409–416.12. Kobbe P, Klemm R, Reilmann H, Hockertz TJ. Less invasive stabilisation system (LISS) for the treatment of periprosthetic femoral fractures: a 3-year follow-up. Injury. 2008; 39(4):472–479.13. Ebraheim NA, Gomez C, Ramineni SK, Liu J. Fixation of periprosthetic femoral shaft fractures adjacent to a well-fixed femoral stem with reversed distal femoral locking plate. J Trauma. 2009; 66(4):1152–1157.14. Bryant GK, Morshed S, Agel J, et al. Isolated locked compression plating for Vancouver Type B1 periprosthetic femoral fractures. Injury. 2009; 40(11):1180–1186.15. Wood GC, Naudie DR, McAuley J, McCalden RW. Locking compression plates for the treatment of periprosthetic femoral fractures around well-fixed total hip and knee implants. J Arthroplasty. 2011; 26(6):886–892.16. Xue H, Tu Y, Cai M, Yang A. Locking compression plate and cerclage band for type B1 periprosthetic femoral fractures preliminary results at average 30-month follow-up. J Arthroplasty. 2011; 26(3):467–471.17. Beals RK, Tower SS. Periprosthetic fractures of the femur: an analysis of 93 fractures. Clin Orthop Relat Res. 1996; (327):238–246.18. Masri BA, Meek RM, Duncan CP. Periprosthetic fractures evaluation and treatment. Clin Orthop Relat Res. 2004; (420):80–95.19. Parvizi J, Vegari DN. Periprosthetic proximal femur fractures: current concepts. J Orthop Trauma. 2011; 25:Suppl 2. S77–S81.20. Parker MJ, Palmer CR. A new mobility score for predicting mortality after hip fracture. J Bone Joint Surg Br. 1993; 75(5):797–798.21. Johansson JE, McBroom R, Barrington TW, Hunter GA. Fracture of the ipsilateral femur in patients wih total hip replacement. J Bone Joint Surg Am. 1981; 63(9):1435–1442.22. Phillips JR, Moran CG, Manktelow AR. Periprosthetic fractures around hip hemiarthroplasty performed for hip fracture. Injury. 2013; 44(6):757–762.23. Brady OH, Garbuz DS, Masri BA, Duncan CP. The reliability and validity of the Vancouver classification of femoral fractures after hip replacement. J Arthroplasty. 2000; 15(1):59–62.24. Park SK, Kim YG, Kim SY. Treatment of periprosthetic femoral fractures in hip arthroplasty. Clin Orthop Surg. 2011; 3(2):101–106.25. Laurer HL, Wutzler S, Possner S, et al. Outcome after operative treatment of Vancouver type B1 and C periprosthetic femoral fractures: open reduction and internal fixation versus revision arthroplasty. Arch Orthop Trauma Surg. 2011; 131(7):983–989.26. Lindahl H, Garellick G, Regner H, Herberts P, Malchau H. Three hundred and twenty-one periprosthetic femoral fractures. J Bone Joint Surg Am. 2006; 88(6):1215–1222.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Treatment of Vancouver B2 and B3 Periprosthetic Femoral Fractures
- Periprosthetic Femoral Fractures after Hip Arthroplasty
- Recurrent Treatment Failure in Vancouver Classification Type C Periprosthetic Fractures around a Well Fixed Short Femoral Stem
- Treatment of Periprosthetic Femoral Fractures after Hip Arthroplasty
- Treatment of Periprosthetic Femoral Fractures after Hip Arthroplasty