Korean J Radiol.
2011 Aug;12(4):519-523. 10.3348/kjr.2011.12.4.519.
MRI Appearance of Prostatic Stromal Sarcoma in a Young Adult
- Affiliations
-
- 1Department of Radiology, Kawasaki Medical School, Okayama 701-0192, Japan. ttamada@med.kawasaki-m.ac.jp
- 2Department of Urology, Kawasaki Medical School, Okayama 701-0192, Japan.
- 3Department of Pathology, Kawasaki Medical School, Okayama 701-0192, Japan.
- KMID: 1783221
- DOI: http://doi.org/10.3348/kjr.2011.12.4.519
Abstract
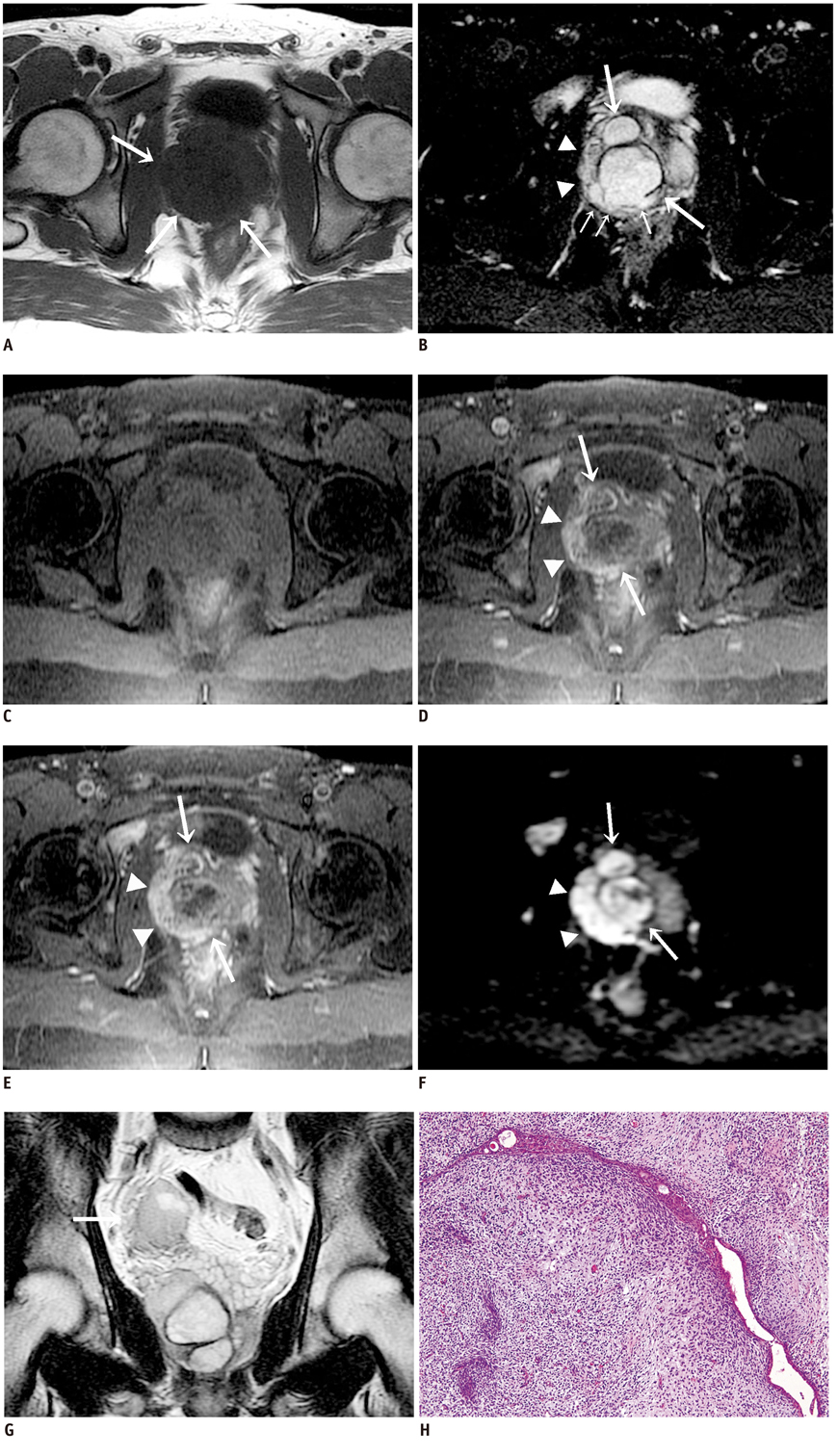
- Prostatic stromal sarcoma (PSS) is quite rare. Herein, we describe magnetic resonance imaging (MRI) features of a PSS identified in a 26-year-old man with dysuria and hematuria. MRI clearly depicted the extent and multinodular appearance of the tumor, which was mainly located in the central zone of the prostate. The tumor appeared as a heterogeneously signal-hyperintense mass with a pseudocapsule on T2-weighted imaging. Contrast-enhanced T1-weighted MRI showed necrotic portions in the gradually enhanced solid mass, and diffusion-weighted imaging permitted the accurate assessment of the local extent of the tumor. Thus, the appearance on MRI was quite different from that of adenocarcinoma of the prostate.
Keyword
MeSH Terms
Figure
Reference
-
1. Chang YS, Chuang CK, Ng KF, Liao SK. Prostatic stromal sarcoma in a young adult: a case report. Arch Androl. 2005. 51:419–424.2. Gaudin PB, Rosai J, Epstein JI. Sarcomas and related proliferative lesions of specialized prostatic stroma: a clinicopathologic study of 22 cases. Am J Surg Pathol. 1998. 22:148–162.3. Morikawa T, Goto A, Tomita K, Tsurumaki Y, Ota S, Kitamura T, et al. Recurrent prostatic stromal sarcoma with massive high-grade prostatic intraepithelial neoplasia. J Clin Pathol. 2007. 60:330–332.4. Probert JL, O'Rourke JS, Farrow R, Cox P. Stromal sarcoma of the prostate. Eur J Surg Oncol. 2000. 26:100–101.5. Huang YC, Wang JY, Lin PY, Chin CC, Chen CS. Synchronous prostate stromal sarcoma and gastrointestinal stromal tumor of rectum: case report and review of the literature. Urology. 2006. 68:672e611–e673.6. Sexton WJ, Lance RE, Reyes AO, Pisters PW, Tu SM, Pisters LL. Adult prostate sarcoma: the M. D. Anderson Cancer Center Experience. J Urol. 2001. 166:521–525.7. Colombo P, Ceresoli GL, Boiocchi L, Taverna G, Grizzi F, Bertuzzi A, et al. Prostatic stromal tumor with fatal outcome in a young man: histopathological and immunohistochemical case presentation. Rare Tumors. 2010. 2:e57.8. Kim JY, Cho YM, Ro JY. Prostatic stromal sarcoma with rhabdoid features. Ann Diagn Pathol. 2010. 14:453–456.9. Fraggetta F, Pepe P, Giunta ML, Aragona F. Primary high grade sarcoma of the specialised prostatic stroma: a case report with clinico-pathological considerations. Pathologica. 2008. 100:482–484.10. Herawi M, Epstein JI. Specialized stromal tumors of the prostate: a clinicopathologic study of 50 cases. Am J Surg Pathol. 2006. 30:694–704.11. Bostwick DG, Hossain D, Qian J, Neumann RM, Yang P, Young RH, et al. Phyllodes tumor of the prostate: long-term followup study of 23 cases. J Urol. 2004. 172:894–899.12. Malhotra P, Bhatia A, Arora VK, Singh N. Pathologic quiz case: a 70-year-old man with bladder outflow obstruction. Prostatic stromal sarcoma. Arch Pathol Lab Med. 2004. 128:e81–e88.13. Osaki M, Takahashi C, Miyagawa T, Adachi H, Ito H. Prostatic stromal sarcoma: case report and review of the literature. Pathol Int. 2003. 53:407–411.14. Froehner M, Bartholdt E, Meye A, Manseck A, Wirth MP. Adult prostate sarcoma diagnosed from tissue spontaneously excreted through the urethra. Urol Oncol. 2004. 22:119–120.15. Sakura M, Tsukamoto T, Yonese J, Ishikawa Y, Aoki N, Fukui I. Successful therapy of a malignant phyllodes tumor of the prostate after postoperative local failure. Urology. 2006. 67:845e811–e843.16. De Raeve H, Jeuris W, Wyndaele JJ, Van Marck E. Cystosarcoma phyllodes of the prostate with rhabdomyoblastic differentiation. Pathol Res Pract. 2001. 197:657–662.17. Cheng YC, Wang JH, Shen SH, Chang YH, Chen PC, Pan CC, et al. MRI findings of prostatic synovial sarcoma. Br J Radiol. 2007. 80:e15–e18.18. Bezzi M, Kressel HY, Allen KS, Schiebler ML, Altman HG, Wein AJ, et al. Prostatic carcinoma: staging with MR imaging at 1.5 T. Radiology. 1988. 169:339–346.19. Tamada T, Sone T, Nagai K, Jo Y, Gyoten M, Imai S, et al. T2-weighted MR imaging of prostate cancer: multishot echo-planar imaging vs fast spin-echo imaging. Eur Radiol. 2004. 14:318–325.20. Akin O, Sala E, Moskowitz CS, Kuroiwa K, Ishill NM, Pucar D, et al. Transition zone prostate cancers: features, detection, localization, and staging at endorectal MR imaging. Radiology. 2006. 239:784–792.21. Tamada T, Sone T, Jo Y, Yamamoto A, Yamashita T, Egashira N, et al. Prostate cancer: relationships between postbiopsy hemorrhage and tumor detectability at MR diagnosis. Radiology. 2008. 248:531–539.22. Bartolozzi C, Selli C, Olmastroni M, Menchi I, Di Candio G. Rhabdomyosarcoma of the prostate: MR findings. AJR Am J Roentgenol. 1988. 150:1333–1334.23. Chang JM, Lee HJ, Lee SE, Byun SS, Choe GY, Kim SH, et al. Pictorial review: Unusual tumours involving the prostate: radiological-pathological findings. Br J Radiol. 2008. 81:907–915.24. Koyama T, Togashi K, Konishi I, Kobayashi H, Ueda H, Kataoka ML, et al. MR imaging of endometrial stromal sarcoma: correlation with pathologic findings. AJR Am J Roentgenol. 1999. 173:767–772.25. Ueda M, Otsuka M, Hatakenaka M, Sakai S, Ono M, Yoshimitsu K, et al. MR imaging findings of uterine endometrial stromal sarcoma: differentiation from endometrial carcinoma. Eur Radiol. 2001. 11:28–33.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Two Different Surgical Approaches for Prostatic Stromal Sarcoma: Robot-Assisted Laparoscopic Radical Prostatectomy and Open Radical Cysto-Prostatectomy With Ileal Conduit
- Two Cases of Low Grade Endometrial Stromal Sarcoma
- Diagnosis of a Gastrointestinal Stromal Tumor Presenting as a Prostatic Mass: A Case Report
- Two Cases of Low-Grade Endometrial Stromal Sarcoma
- A Case of Low-Grade Endometrial Stromal Sarcoma of the Uterus (So-Called ""Endolymphatic Stromal Myosis"")