Outcome of Endovascular Treatment in Symptomatic Intracranial Vascular Stenosis
- Affiliations
-
- 1Department of Radiology, Asan Medical Center, University of Ulsan College of Medicine, Korea. dcsuh@www.amc.seoul.kr
- 2Department of Neurology, Asan Medical Center, University of Ulsan College of Medicine, Korea.
- 3Department of Emergency Medicine, Asan Medical Center, University of Ulsan College of Medicine, Korea.
- 4Department of Radiology, DaeJeon Catholic Hospital, Korea.
- KMID: 1783166
- DOI: http://doi.org/10.3348/kjr.2005.6.1.1
Abstract
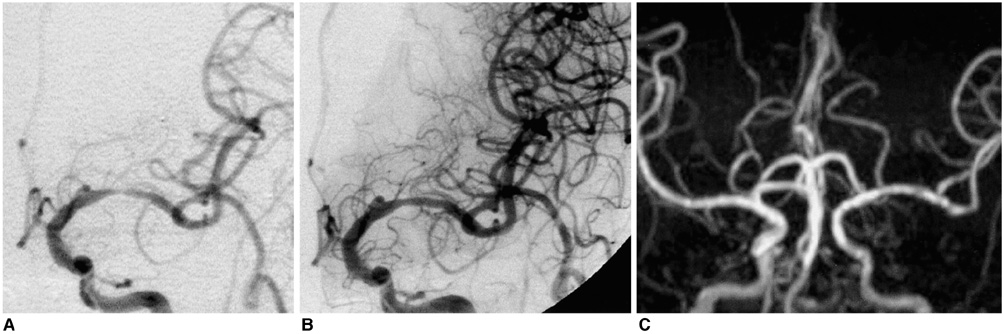
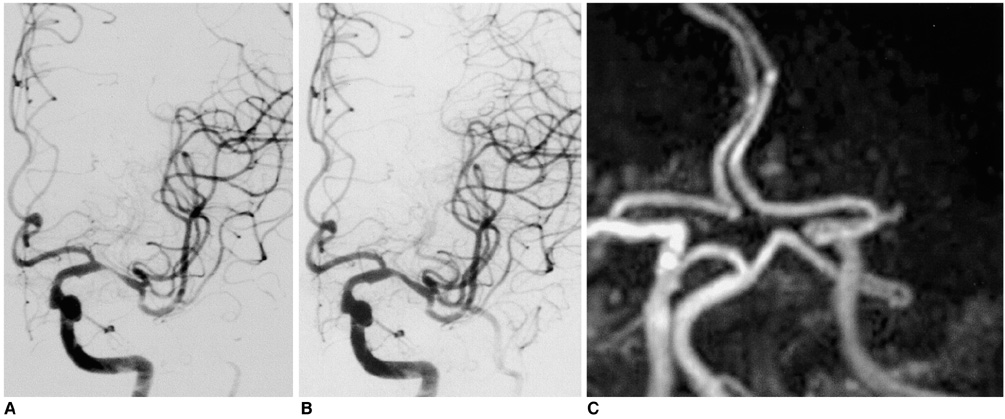
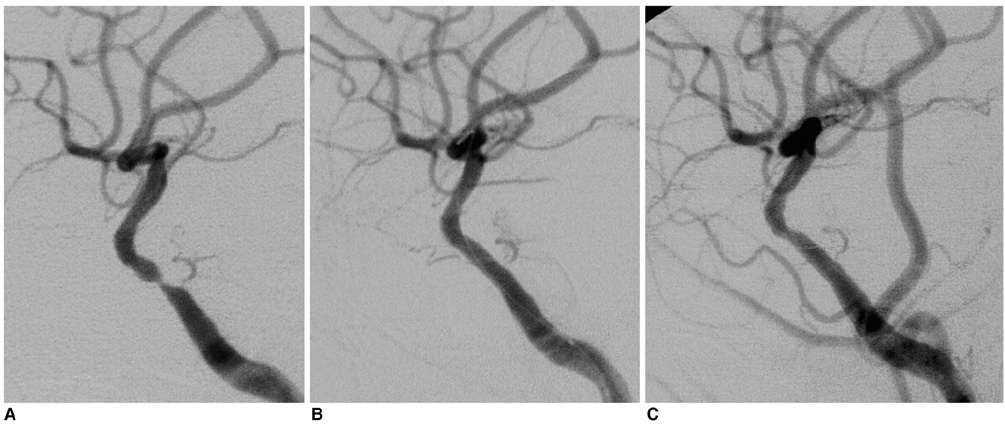
OBJECTIVE
The outcome evaluation for the revascularization of intracranial vascular stenoses has not been fully described due to the highly technical nature of the procedure. We report here on the early and late clinical outcomes of angioplasty and/or stenting of symptomatic severe intracranial vascular stenoses at a single institute. MATERIALS AND METHODS: Since 1995, we have treated 35 patients with symptomatic intracranial vascular stenosis (more than 70% stenosis, mean stenosis: 78.6%+/-6.2%). An gioplasty (n = 19) was performed for the horizontal segment of the middle cerebral artery (M1) (n = 16) and the basilar artery (BA) (n = 1), the intradural vertebral artery (VA) (n = 1), and the cavernous internal carotid artery (ICA) (n = 1). Stenting (n = 16) was performed for the cavernous or petrous ICAs (n = 9), the intradural VA (n = 3), BA (n = 2), and M1 (n = 2) artery. We assessed the angiographic success (defined as residual stenosis < 50%) rate, the periprocedural complications during the 30-day periprocedural period, the symptomatic recurrence and restenosis during a mean 22-month follow-up (FU) period. The Kaplan-Meier estimate of the cumulative event-free rate of the major cerebrovascular events, i.e. death, stroke or restenosis, was also done. RESULTS: Angiographic success was achieved in 97% of our patients (34/35). There were four procedure-related complications (11%) including a death and a minor stroke. During the mean 22-month FU, the asymptomatic restenosis rate was 9% and the symptomatic restenosis rate was 6% in the target lesion and 9% in all the vascular territories. The Kaplan-Meier estimate was 70.6% (95% confidence interval = 46.5-94.7) after 33 months of FU. CONCLUSION: In addition to a high angiographic success rate and an acceptable periprocedural complication rate, intracranial angioplasty and/or stenting revealed a relatively low symptomatic recurrence rate. Hemorrhage is a rare, but the physician must aware that potentially fatal periprocedural complications can occur.
MeSH Terms
Figure
Cited by 5 articles
-
An update on interventional revascularization therapy of intracranial arterial steno-occlusive diseases
Deok Hee Lee
J Korean Med Assoc. 2012;55(9):869-877. doi: 10.5124/jkma.2012.55.9.869.Intracranial Atherosclerosis: Incidence, Diagnosis and Treatment
Jong S. Kim, Dong-Wha Kang, Sun U. Kwon
J Clin Neurol. 2005;1(1):1-7. doi: 10.3988/jcn.2005.1.1.1.Mechanism of Procedural Failure Related to Wingspan
Lin-Bo Zhao, Soonchan Park, Donggeun Lee, Deok Hee Lee, Dae Chul Suh
Neurointervention. 2012;7(2):102-108. doi: 10.5469/neuroint.2012.7.2.102.Change of Platelet Reactivity to Antiplatelet Therapy after Stenting Procedure for Cerebral Artery Stenosis: VerifyNow Antiplatelet Assay before and after Stenting
Deok Hee Lee, Ho Sung Kim, Sun Mi Kim, Sun-Uck Kwon, Dae Chul Suh
Neurointervention. 2012;7(1):23-26. doi: 10.5469/neuroint.2012.7.1.23.Long-term Outcomes of Drug-eluting Stents in Symptomatic Intracranial Stenosis
Soonchan Park, Dong-geun Lee, Won-Jung Chung, Deok Hee Lee, Dae Chul Suh
Neurointervention. 2013;8(1):9-14. doi: 10.5469/neuroint.2013.8.1.9.
Reference
-
1. Sacco RL, Kargman DE, Gu Q, Zamanillo MC. Race-ethnicity and determinants of intracranial atherosclerotic cerebral infarction. The Northern Manhattan Stroke Study. Stroke. 1995. 26:14–20.2. Wityk RJ, Lehman D, Klag M, Coresh J, Ahn H, Litt B. Race and sex differences in the distribution of cerebral atherosclerosis. Stroke. 1996. 27:1974–1980.3. Suh DC, Lee SH, Kim KR, Park ST, Lim SM, Kim SJ, et al. Pattern of atherosclerotic carotid stenosis in Korean patients with stroke: different involvement of intracranial versus extracranial vessels. AJNR Am J Neuroradiol. 2003. 24:239–244.4. Lee SJ, Cho SJ, Moon HS, Shon YM, Lee KH, Kim DI, et al. Combined extracranial and intracranial atherosclerosis in Korean patients. Arch Neurol. 2003. 60:1561–1564.5. Warfarin-Aspirin Symptomatic Intracranial Disease (WASID) Trial Investigators. Design, progress and challenges of a double-blind trial of warfarin versus aspirin for symptomatic intracranial arterial stenosis. Neuroepidemiology. 2003. 22:106–117.6. Chimowitz MI, Kokkinos J, Strong J, Brown MB, Levine SR, Silliman S, et al. The Warfarin-Aspirin Symptomatic Intracranial Disease Study. Neurology. 1995. 45:1488–1493.7. The Warfarin-Aspirin Symptomatic Intracranial Disease (WASID) Study Group. Prognosis of patients with symptomatic vertebral or basilar artery stenosis. Stroke. 1998. 29:1389–1392.8. Thijs VN, Albers GW. Symptomatic intracranial atherosclerosis: outcome of patients who fail antithrombotic therapy. Neurology. 2000. 55:490–497.9. The EC/IC Bypass Study Group. Failure of extracranial-intracranial arterial bypass to reduce the risk of ischemic stroke. Results of an international randomized trial. N Engl J Med. 1985. 313:1191–1200.10. Ausman JI, Diaz FG, Vacca DF, Sadasivan B. Superficial temporal and occipital artery bypass pedicles to superior, anterior inferior, and posterior inferior cerebellar arteries for vertebrobasilar insufficiency. J Neurosurg. 1990. 72:554–558.11. Chaturvedi S, St Pierre ME, Bertasio B. Cerebral angioplasty practice at major medical centers in the United States. Neuroradiology. 2000. 42:218–220.12. Takis C, Kwan ES, Pessin MS, Jacobs DH, Caplan LR. Intracranial angioplasty: experience and complications. AJNR Am J Neuroradiol. 1997. 18:1661–1668.13. Mori T, Fukuoka M, Kazita K, Mori K. Follow-up study after intracranial percutaneous transluminal cerebral balloon angioplasty. AJNR Am J Neuroradiol. 1998. 19:1525–1533.14. Suh DC, Sung KB, Cho YS, Choi CG, Lee HK, Lee JH, et al. Transluminal angioplasty for middle cerebral artery stenosis in patients with acute ischemic stroke. AJNR Am J Neuroradiol. 1999. 20:553–558.15. Marks MP, Marcellus M, Norbash AM, Steinberg GK, Tong D, Albers GW. Outcome of angioplasty for atherosclerotic intracranial stenosis. Stroke. 1999. 30:1065–1069.16. Nahser HC, Henkes H, Weber W, Berg-Dammer E, Yousry TA, Kuhne D. Intracranial vertebrobasilar stenosis: angioplasty and follow-up. AJNR Am J Neuroradiol. 2000. 21:1293–1301.17. Gomez CR, Misra VK, Liu MW, Wadlington VR, Terry JB, Tulyapronchote R, et al. Elective stenting of symptomatic basilar artery stenosis. Stroke. 2000. 31:95–99.18. Levy EI, Horowitz MB, Koebbe CJ, Jungreis CC, Pride GL, Dutton K, et al. Transluminal stent-assisted angiplasty of the intracranial vertebrobasilar system for medically refractory, posterior circulation ischemia: early results. Neurosurgery. 2001. 48:1215–1221.19. Lylyk P, Cohen JE, Ceratto R, Ferrario A, Miranda C. Angioplasty and stent placement in intracranial atherosclerotic stenoses and dissections. AJNR Am J Neuroradiol. 2002. 23:430–436.20. Levy EI, Hanel RA, Bendok BR, Boulos AS, Hartney ML, Guterman LR, et al. Staged stent-assisted angioplasty for symptomatic intracranial vertebrobasilar artery stenosis. J Neurosurg. 2002. 97:1294–1301.21. Gupta R, Schumacher HC, Mangla S, Meyers PM, Duong H, Khandji AG, et al. Urgent endovascular revascularization for symptomatic intracranial atherosclerotic stenosis. Neurology. 2003. 61:1729–1735.22. Levy EI, Hanel RA, Boulos AS, Bendok BR, Kim SH, Gibbons KJ, et al. Comparison of periprocedure complications resulting from direct stent placement compared with those due to conventional and staged stent placement in the basilar artery. J Neurosurg. 2003. 99:653–660.23. de Rochemont Rdu M, Turowski B, Buchkremer M, Sitzer M, Zanella FE, Berkefeld J. Recurrent symptomatic high-grade intracranial stenoses: safety and efficacy of undersized stents--initial experience. Radiology. 2004. 231:45–49.24. Lee JH, Kwon SU, Suh DC, Kim JS. Percutaneous transluminal angioplasty for symptomatic middle cerebral artery stenosis: long-term follow-up. Cerebrovasc Dis. 2003. 15:90–97.25. Barnett HJ, Taylor DW, Eliasziw M, Fox AJ, Ferguson GG, Haynes RB, et al. Benefit of carotid endarterectomy in patients with symptomatic moderate or severe stenosis. North American Symptomatic Carotid Endarterectomy Trial Collaborators. N Engl J Med. 1998. 339:1415–1425.26. Baumgartner RW, Mattle HP, Schroth G. Assessment of >/=50% and < 50% intracranial stenoses by transcranial color-coded duplex sonography. Stroke. 1999. 30:87–92.27. Goldstein LB, Samsa GP. Reliability of the National Institutes of Health Stroke Scale. Extension to non-neurologists in the context of a clinical trial. Stroke. 1997. 28:307–310.28. Dangas G, Fuster V. Management of restenosis after coronary intervention. Am Heart J. 1996. 132:428–436.29. Aliabadi D, Tilli FV, Bowers TR, Benzuly KH, Safian RD, Goldstein JA, et al. Incidence and angiographic predictors of side branch occlusion following high-pressure intracoronary stenting. Am J Cardiol. 1997. 80:994–997.30. Cho GY, Lee CW, Hong MK, Kim JJ, Park SW, Park SJ. Effects of stent design on side branch occlusion after coronary stent placement. Catheter Cardiovasc Interv. 2001. 52:18–23.31. Wakhloo AK, Tio FO, Lieber BB, Schellhammer F, Graf M, Hopkins LN. Self-expanding nitinol stents in canine vertebral arteries: hemodynamics and tissue response. AJNR Am J Neuroradiol. 1995. 16:1043–1051.32. Lopes DK, Ringer AJ, Boulos AS, Qureshi AI, Lieber BB, Guterman LR, et al. Fate of branch arteries after intracranial stenting. Neurosurgery. 2003. 52:1275–1278. discussion 1278-1279.33. Jiang WJ, Wang YJ, Du B, Wang SX, Wang GH, Jin M, et al. Stenting of symptomatic M1 stenosis of middle cerebral artery: an initial experience of 40 patients. Stroke. 2004. 35:1375–1380.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Guideline for Intracranial Stenting of Symptomatic Intracranial Artery Stenosis: Preliminary Report
- Angioplasty, Stenting and Other Potential Treatments of Atherosclerotic Stenosis of the Intracranial Arteries: Past, Present and Future
- Endovascular treatment of intracranial aneurysms: Past and present
- In-Stent Stenosis of Stent Assisted Endovascular Treatment on Intracranial Complex Aneurysms
- Vascular Perforation During Coil Embolization of an Intracranial Aneurysm: the Incidence, Mechanism, and Clinical Outcome