Yonsei Med J.
2009 Feb;50(1):83-88. 10.3349/ymj.2009.50.1.83.
How Well Does the Target INR Level Maintain in Warfarin-Treated Patients with Non-ValvularAtrial Fibrillation?
- Affiliations
-
- 1Division of Cardiology, Department of Medicine, Cardiac and Vascular Center, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea. juneskim@skku.edu
- 2Department of Medicine, The Armed Forced Seoul Hospital, Seoul, Korea.
- KMID: 1782972
- DOI: http://doi.org/10.3349/ymj.2009.50.1.83
Abstract
- PURPOSE
Although warfarin is an effective oral anticoagulation (OAC) drug to reduce the risk of thromboembolism in patients with non-valvular atrial fibrillation (NVAF), long term follow-up data are scarce to be certain whether the target INR level is maintained in warfarin-treated patients in Korea. The aim of this study was to evaluate how well INRs are maintained within the target range using a new index, INR stability (= 100 x number of INRs within target range/total number of INR measurements) which we made, and to find out any correlation between thromboembolic events and INR stability.
MATERIALS AND METHODS
This study was an observational analysis of retrospectively collected data of 129 patients with NVAF from April 2000 to December 2005 at a single tertiary hospital. All patients were registered at the anticoagulation service.
RESULTS
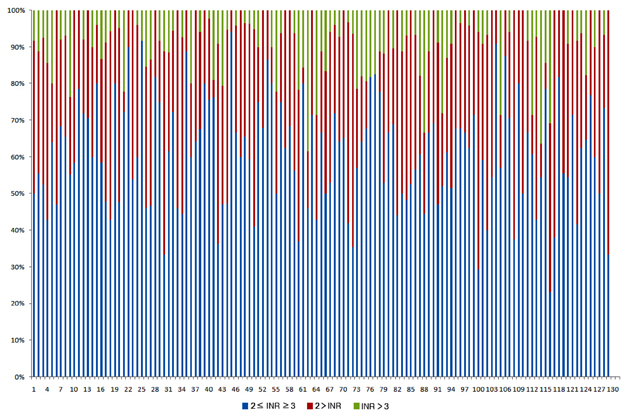
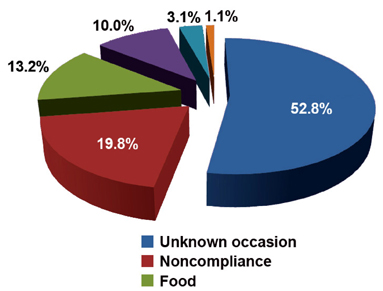
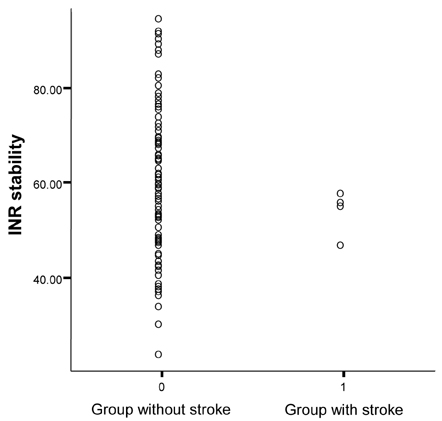
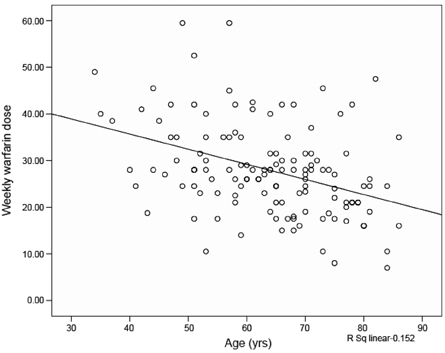
The median duration of follow up was 2.03 years (interquartile range 1.35 - 2.96). During the follow-up period, 60.9 +/- 14.9% of the INR were within the target INR range. INR stability was not significantly different between patients without and with stroke (61.2 +/- 15.0% vs 53.3 +/- 4.9%). Among the known factors affecting fluctuations of the INR value, the most frequent factor was noncompliance (41.8%).
CONCLUSION
The present study showed that it was not enough to maintain INR values within the target range in warfarin-treated patients with NVAF even at a tertiary hospital. Noncompliance is an important problem which interferes with maintaining target INR range.
Keyword
MeSH Terms
-
Adult
Age Factors
Aged
Aged, 80 and over
Anticoagulants/*therapeutic use
Atrial Fibrillation/*drug therapy/epidemiology/etiology
Drug Monitoring/methods
Female
Follow-Up Studies
Heart Valves
Humans
*International Normalized Ratio
Male
Middle Aged
Patient Compliance
Retrospective Studies
Risk Factors
Thrombosis/*blood/epidemiology/*prevention & control
Warfarin/*therapeutic use
Figure
Reference
-
1. Wolf PA, Abbott RD, Kannel WB. Atrial fibrillation as an independent risk factor for stroke: the Framingham Study. Stroke. 1991. 22:983–988.
Article2. Risk factors for stroke and efficacy of antithrombotic therapy in atrial fibrillation. Analysis of pooled data from five randomized controlled trials. Arch Intern Med. 1994. 154:1449–1457.3. Ezekowitz MD, Bridgers SL, James KE, Carliner NH, Colling CL, Gornick CC, et al. Warfarin in the prevention of stroke associated with nonrheumatic atrial fibrillation. Veterans Affairs Stroke Prevention in Nonrheumatic Atrial Fibrillation Investigators. N Engl J Med. 1992. 327:1406–1412.
Article4. Connolly SJ, Laupacis A, Gent M, Roberts RS, Cairns JA, Joyner C. Canadian Atrial Fibrillation Anticoagulation (CAFA) Study. J Am Coll Cardiol. 1991. 18:349–355.5. Stroke Prevention in Atrial Fibrillation Study. Final results. Circulation. 1991. 84:527–539.6. The effect of low-dose warfarin on the risk of stroke in patients with nonrheumatic atrial fibrillation. The Boston Area Anticoagulation Trial for Atrial Fibrillation Investigators. N Engl J Med. 1990. 323:1505–1511.7. Petersen P, Boysen G, Godtfredsen J, Andersen ED, Andersen B. Placebo-controlled, randomised trial of warfarin and aspirin for prevention of thromboembolic complications in chronic atrial fibrillation. The Copenhagen AFASAK study. Lancet. 1989. 1:175–179.8. Aronow WS, Ahn C, Kronzon I, Gutstein H. Risk factors for new thromboembolic stroke in patients > or = 62 years of age with chronic atrial fibrillation. Am J Cardiol. 1998. 82:119–121.9. Koefoed BG, Gulløv AL, Petersen P. Prevention of thromboembolic events in atrial fibrillation. Thromb Haemost. 1997. 78:377–381.
Article10. Lip GY, Lowe GD. ABC of atrial fibrillation. Antithrombotic treatment for atrial fibrillation. BMJ. 1996. 312:45–49.
Article11. Predictors of thromboembolism in atrial fibrillation: I. Clinical features of patients at risk. The Stroke Prevention in Atrial Fibrillation Investigators. Ann Intern Med. 1992. 116:1–5.12. Wolf PA, Dawber TR, Thomas HE Jr, Kannel WB. Epidemiologic assessment of chronic atrial fibrillation and risk of stroke: the Framingham study. Neurology. 1978. 28:973–977.
Article13. Hylek EM, Go AS, Chang Y, Jensvold NG, Henault LE, Selby JV, et al. Effect of intensity of oral anticoagulation on stroke severity and mortality in atrial fibrillation. N Engl J Med. 2003. 349:1019–1026.
Article14. Hirsh J, Fuster V, Ansell J, Halperin JL. American Heart Association. American College of Cardiology Foundation. American Heart Association/American College of Cardiology Foundation guide to warfarin therapy. Circulation. 2003. 107:1692–1711.
Article15. Samsa GP, Matchar DB, Goldstein LB, Bonito AJ, Lux LJ, Witter DM, et al. Quality of anticoagulation management among patients with atrial fibrillation: results of a review of medical records from 2 communities. Arch Intern Med. 2000. 160:967–973.
Article16. Jones M, McEwan P, Morgan CL, Peters JR, Goodfellow J, Currie CJ. Evaluation of the pattern of treatment, level of anticoagulation control, and outcome of treatment with warfarin in patients with non-valvar atrial fibrillation: a record linkage study in a large British population. Heart. 2005. 91:472–477.
Article17. Bungard TJ, Ghali WA, Teo KK, McAlister FA, Tsuyuki RT. Why do patients with atrial fibrillation not receive warfarin? Arch Intern Med. 2000. 160:41–46.
Article18. Holbrook AM, Pereira JA, Labiris R, McDonald H, Douketis JD, Crowther M, et al. Systematic overview of warfarin and its drug and food interactions. Arch Intern Med. 2005. 165:1095–1106.
Article19. Rosendaal FR, Cannegieter SC, van der Meer FJ, Briét E. A method to determine the optimal intensity of oral anticoagulant therapy. Thromb Haemost. 1993. 69:236–239.
Article20. Garcia D, Regan S, Crowther M, Hughes RA, Hylek EM. Warfarin maintenance dosing patterns in clinical practice: implications for safer anticoagulation in the elderly population. Chest. 2005. 127:2049–2056.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Clinical Utility and Accuracy of Coaguchek(R) XS, a Reliable Alternative to Laboratory International Normalized Ratio Monitoring in Korean Patients With Atrial Fibrillation
- Optimal International Normalized Ratio for Warfarin Therapy in Elderly Korean Patients with Non-Valvular Atrial Fibrillation
- Impact of Anticoagulation Intensity in Korean Patients with Atrial Fibrillation: Is It Different from Western Population?
- Determination of Plasma Warfarin Concentrations in Korean Patients and Its Potential for Clinical Application
- Trends in Oral Anticoagulation Therapy Among Korean Patients With Atrial Fibrillation: The KORean Atrial Fibrillation Investigation