J Korean Med Sci.
2012 Sep;27(9):1105-1108. 10.3346/jkms.2012.27.9.1105.
Meningitis by Toxocara canis after Ingestion of Raw Ostrich Liver
- Affiliations
-
- 1Department of Neurology, Sungkyunkwan University School of Medicine, Samsung Medical Center, Seoul, Korea.
- 2Department of Parasitology and Tropical Medicine, Institute of Endemic Diseases, Seoul National University College of Medicine, Seoul, Korea.
- 3Department of Neurology, Ewha Womans University Medical Center, Seoul, Korea.
- 4Department of Neurology and Movement Disorder Center, Seoul National University Hospital, Seoul National University College of Medicine, Seoul, Korea. brain@snu.ac.kr
- KMID: 1782147
- DOI: http://doi.org/10.3346/jkms.2012.27.9.1105
Abstract
- Recently reports on toxocariasis are increasing by serodiagnosis in Korea. A previously healthy 17-yr-old boy complained of headache, fever, dyspnea, and anorexia. He showed symptoms and signs of eosinophilic meningitis with involvement of the lungs and liver. Specific IgG antibody to Toxocara canis larval antigen was positive in serum and cerebrospinal fluid by ELISA. He took raw ostrich liver with his parents 4 weeks before the symptom onset. His parents were seropositive for T. canis antigen but had no symptoms or signs suggesting toxocariasis. This is the first report of toxocariasis in a family due to ingestion of raw ostrich liver in Korea.
Keyword
MeSH Terms
-
Adolescent
Animals
Antibodies, Helminth/blood/cerebrospinal fluid
Eating
Humans
Larva/immunology
Liver/parasitology
Male
Meningitis/*diagnosis/parasitology
Struthioniformes
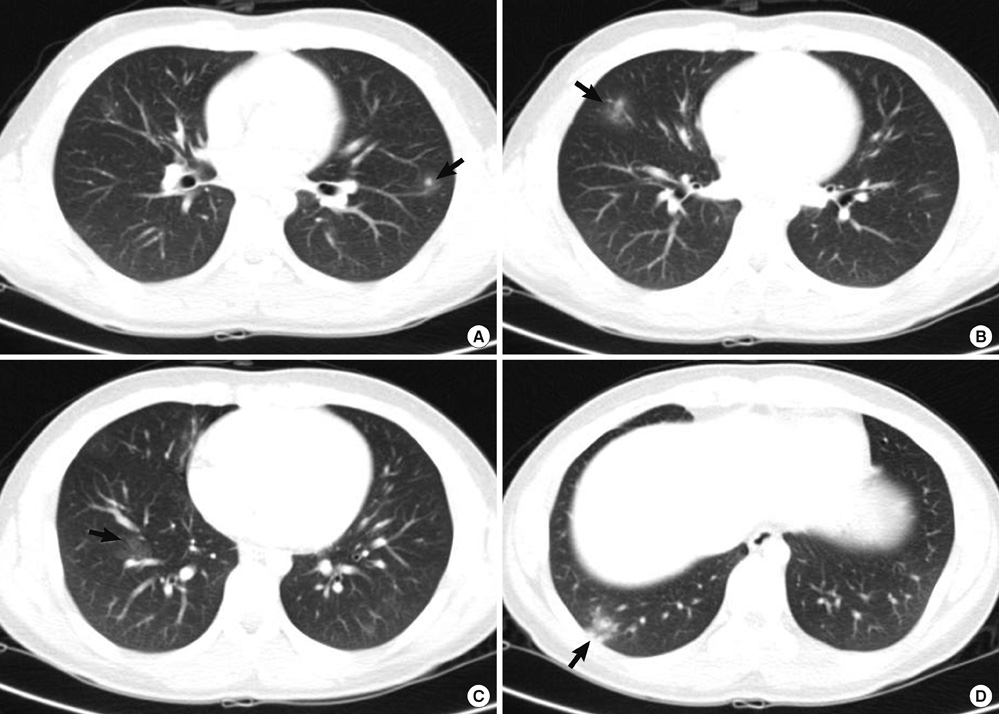
Tomography, X-Ray Computed
Toxocara canis/growth & development/*immunology/isolation & purification
Toxocariasis/*diagnosis/parasitology/transmission
Antibodies, Helminth
Figure
Cited by 2 articles
-
Clinical Manifestation of Eosinophilic Meningitis in Korean Children: A Single Institution's Experience
Jung Hee Byun, Seong Yeol Choi, Dong Soo Kim, Ki Hwan Kim
Pediatr Infect Vaccine. 2015;22(1):23-28. doi: 10.14776/piv.2015.22.1.23.Eosinophilic Meningitis Associated with Toxocariasis
Jin Kyo Choi, Jin Woo Lee, Yong Hui Park, Seo Hyun Kim
J Neurocrit Care. 2015;8(2):115-117. doi: 10.18700/jnc.2015.8.2.115.
Reference
-
1. Finsterer J, Auer H. Neurotoxocariasis. Rev Inst Med Trop Sao Paulo. 2007. 49:279–287.2. Graeff-Teixeira C, da Silva AD, Yoshimura K. Update on eosinophilicc meningoencephalitis and its clinical relevance. Clin Microbiol Rev. 2009. 22:322–348.3. Choi D, Lim JH, Choi DC, Paik SW, Kim SH, Huh S. Toxocariasis and ingestion of raw cow liver in patients with eosinophilia. Korean J Parasitol. 2008. 46:139–143.4. Nagakura K, Tachibana H, Kaneda Y, Keto Y. Toxocariasis possibly caused by ingesting raw chicken. J Infect Dis. 1989. 160:735–736.5. Sturchler D, Weiss N, Gassner M. Transmission of toxocariasis. J Infect Dis. 1990. 162:571.6. Overgaauw PA. Aspects of Toxocara epidemiology: human toxocariosis. Crit Rev Microbiol. 1997. 23:215–231.7. Haralambidou S, Vlacheaki E, Ioannidou E, Milioni V, Haralambidis S, Klonizakis I. Pulmonary and myocardial manifestations due to Toxocara canis infection. Eur J Intern Med. 2005. 16:601–602.8. Lim JH. Foodborne eosinophilia due to visceral larva migrans: a disease abandoned. J Korean Med Sci. 2012. 27:1–2.9. Park HY, Lee SU, Huh S, Kong Y, Magnaval JF. A seroepidemiological survey for toxocariasis in apparently healthy residents in Gangwon-do, Korea. Korean J Parasitol. 2002. 40:113–117.10. Yoon YS, Lee CH, Kang YA, Kwon SY, Yoon HI, Lee JH, Lee CH. Impact of toxocariasis in patients with unexplained patchy pulmonary infiltrate in Korea. J Korean Med Sci. 2009. 24:40–45.11. Taylor MR, Keane CT, O'Connor P, Girdwood RW, Smith H. Clinical features of covert toxocariasis. Scand J Infect Dis. 1987. 19:693–696.12. Magnaval JF, Glickman LT, Dorchies P, Morassin B. Highlights of human toxocariasis. Korean J Parasitol. 2001. 39:1–11.13. Xinou E, Lefkopoulos A, Gelagoti M, Drevelegas A, Diaakou A, Milonas I, Dimitriadis AS. CT and MR imaging findings in cerebral toxocaral disease. AJNR Am J Neuroradiol. 2003. 24:714–718.14. Glickman L, Summers BA. Experimental Toxocara canis infection in Cynomolgus macaques (Macaca fascicularis). Am J Vet Res. 1983. 44:2347–2354.15. Good B, Holland CV, Stafford P. The influence of inoculum size and time post-infection on the number and position of Toxocara canis larvae recovered from the brains of outbred CD1 mice. J Helminthol. 2001. 75:175–181.16. Fan CK, Lin YH, Du WY, Su KE. Infectivity and pathogenicity of 14-month-cultured embryonated eggs of Toxocara canis in mice. Vet Parasitol. 2003. 113:145–155.17. Vidal JE, Sztajnbok J, Seguro AC. Eosinophilic meningoencephalitis due to Toxocara canis: case report and review of the literature. Am J Trop Med Hyg. 2003. 69:341–343.18. Eberhardt O, Bialek R, Nagele R, Dichgans J. Eosinophilic meningomyelitis in toxocariasis: case report and review of the literature. Clin Neurol Neurosurg. 2005. 107:432–438.19. Despommier D. Toxocariasis: clinical aspects, epidemiology, medical ecology, and molecular aspects. Clin Microbiol Rev. 2003. 16:265–272.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Severe Hypereosinophilia Caused by Toxocara Infection after Ingestion of Raw Ostrich Liver
- Transmission of Toxocara canis via Ingestion of Raw Cow Liver: A Cross-Sectional Study in Healthy Adults
- Familial Case of Visceral Larval Migrans of Toxocara Canis after Ingestion of Raw Chicken Liver
- A case of Visceral Larva Migrans Due to Toxocara Carni in the Emergency Department
- A Case of Pulmonary Infiltration with Eosinophilia in Visceral Larval Migrans by Toxocara Canis