Trends in Epidemiology of Neonatal Sepsis in a Tertiary Center in Korea: A 26-Year Longitudinal Analysis, 1980-2005
- Affiliations
-
- 1Department of Pediatrics, Inje University Sanggye Paik Hospital, Seoul, Korea.
- 2Department of Pediatrics, Seoul National University College of Medicine, Seoul, Korea. kimhans@snu.ac.kr
- 3Department of Pediatrics, Sungkyunkwan University School of Medicine, Samsung Medical Center, Seoul, Korea.
- KMID: 1782120
- DOI: http://doi.org/10.3346/jkms.2011.26.2.284
Abstract
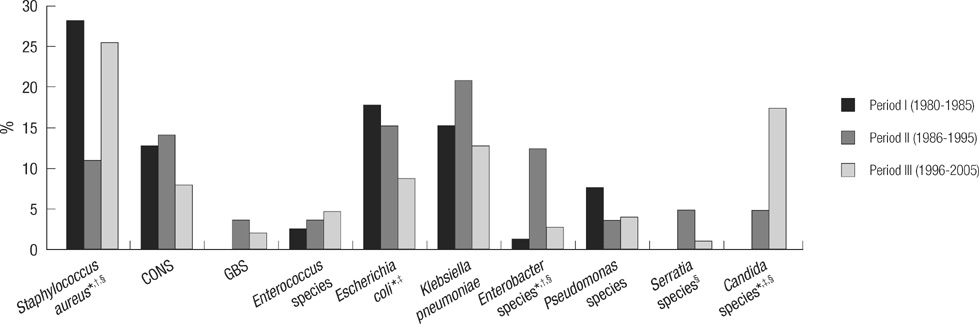
- There were many reports of longitudinal changes in the causative organisms of neonatal sepsis in Western countries but few in Asia. We aimed to study longitudinal trends in the epidemiology of neonatal sepsis at Seoul National University Children's Hospital (SNUCH), a tertiary center in Korea, and compared the results to previous studies of Western countries. The medical records of all of the neonates who were hospitalized at SNUCH from 1996 to 2005 with positive blood cultures were reviewed. We also compared the findings to previous 16-yr (1980-1995). One hundred and forty-nine organisms were identified in 147 episodes from 134 infants. In comparison with the previous 16-yr studies, there was a decrease in the number of Escherichia coli infections (16.2% vs 8.7%: odds ratio [OR] 0.495; 95% confidence interval [CI], 0.255-0.962; P = 0.035), but an increase in Staphylococcus aureus (16.6% vs 25.5%: OR 1.720; 95% CI, 1.043-2.839; P = 0.033) and fungal infections (3.3% vs 18.7%: OR 6.740; 95% CI, 2.981-15.239; P < 0.001), predominantly caused by Candida species. In conclusion, the incidence of sepsis caused by E. coli decreases, but S. aureus and fungal sepsis increases significantly. Compared with Western studies, the incidence of sepsis caused by S. aureus and fungus has remarkably increased.
Keyword
MeSH Terms
Figure
Cited by 5 articles
-
A Case of Neonatal Meningitis Caused by Streptococcus dysgalactiae subspecies dysgalactiae and Herpes Simplex Virus
Geeyae Im, Yoonseon Park, Minsung Kim, Ki Hwan Kim, Sang Yong Kim, Seung Yun Chung
Pediatr Infect Vaccine. 2019;26(3):194-198. doi: 10.14776/piv.2019.26.e17.Usefulness of a Rapid Real-time PCR Assay in Prenatal Screening for Group B Streptococcus Colonization
Jeong Su Park, Dong-Hee Cho, Jae Hyug Yang, Moon Young Kim, Son Moon Shin, Eui-Chong Kim, Sung Sup Park, Moon-Woo Seong
Ann Lab Med. 2013;33(1):39-44. doi: 10.3343/alm.2013.33.1.39.1차 분만병원 수준에서의 임신 후기 산모의질내 B군 연쇄상 구균 집락 형성의 임상적 특성에 대한 평가
Sumin Oh, Joong Shin Park
J Korean Soc Matern Child Health. 2022;26(1):27-34. doi: 10.21896/jksmch.2022.26.1.27.Group B Streptococcal Meningitis in Neonate: 2001-2011
Jiin Cheong, Shin-yun Byun, Myo-Jing Kim
Korean J Perinatol. 2013;24(3):142-147. doi: 10.14734/kjp.2013.42.2.142.국내 3차 의료기관에서의 신생아 조기 발병 B군 사슬알균 감염증 역학: 2001-2022년, 22년간의 종단 연구
Hyeongyu Lee, Kwangjin Ahn, Jieun Kang, Seong Jin Choi, Yeong Myong Yoo, Young Uh
Lab Med Online. 2025;15(1):78-83. doi: 10.47429/lmo.2025.15.1.78.
Reference
-
1. Bizzarro MJ, Raskind C, Baltimore RS, Gallagher PG. Seventy-five years of neonatal sepsis at Yale: 1928-2003. Pediatrics. 2005. 116:595–602.2. Stoll BJ, Hansen N, Fanaroff AA, Wright LL, Carlo WA, Ehrenkranz RA, Lemons JA, Donovan EF, Stark AR, Tyson JE, Oh W, Bauer CR, Korones SB, Shankaran S, Laptook AR, Stevenson DK, Papile LA, Poole WK. Late-onset sepsis in very low birth weight neonates: the experience of the NICHD Neonatal Research Network. Pediatrics. 2002. 110:285–291.3. Vesikari T, Janas M, Grönroos P, Tuppurainen N, Renlund M, Kero P, Koivisto M, Kunnas M, Heinonen K, Nyman R, Pettay O, Osterlund K. Neonatal septicaemia. Arch Dis Child. 1985. 60:542–546.4. Rønnestad A, Abrahamsen TG, Gaustad P, Finne PH. Blood culture isolates during 6 years in a tertiary neonatal intensive care unit. Scand J Infect Dis. 1998. 30:245–251.5. Butler KM, Baker CJ. Candida: an increasingly important pathogen in the nursery. Pediatr Clin North Am. 1988. 35:543–563.6. Rangel-Frausto MS, Wiblin T, Blumberg HM, Saiman L, Patterson J, Rinaldi M, Pfaller M, Edwards JE Jr, Jarvis W, Dawson J, Wenzel RP. National epidemiology of mycoses survey (NEMIS): variations in rates of bloodstream infections due to Candida species in seven surgical intensive care units and six neonatal intensive care units. Clin Infect Dis. 1999. 29:253–258.7. Fridkin SK, Kaufman D, Edwards JR, Shetty S, Horan T. Changing incidence of Candida bloodstream infections among NICU patients in the United States: 1995-2004. Pediatrics. 2006. 117:1680–1687.8. Garner JS, Jarvis WR, Emori TG, Horan TC, Hughes JM. CDC definitions for nosocomial infections, 1988. Am J Infect Control. 1988. 16:128–140.9. Tessin I, Trollfors B, Thiringer K. Incidence and etiology of neonatal septicaemia and meningitis in western Sweden 1975-1986. Acta Paediatr Scand. 1990. 79:1023–1030.10. Hervás JA, Alomar A, Salvá F, Reina J, Benedí VJ. Neonatal sepsis and meningitis in Mallorca, Spain, 1977-1991. Clin Infect Dis. 1993. 16:719–724.11. Persson E, Trollfors B, Brandberg LL, Tessin I. Septicaemia and meningitis in neonates and during early infancy in the Göteborg area of Sweden. Acta Paediatr. 2002. 91:1087–1092.12. Kim KA, Shin SM, Choi JH. A nationwide survey on the causative organisms of neonatal sepsis in Korea. J Korean Pediatr Soc. 2002. 45:55–63.13. Kim TH, Park SE, Kim KH. A study of group B streptococcal infection in pregnant women, by LIM broth media. Korean J Pediatr. 2004. 47:1072–1075.14. Choi KU, Koh SK, Lee JY, Park JH, Hwang SO, Lee BI, Lee WY. Clinical significance of group B streptococcal infection in pregnant women. Korean J Obstet Gynecol. 2002. 45:811–815.15. Park HW, Lim G, Koo SE, Lee BS, Kim KS, Pi SY, Kim AR. Causative agents and antimicrobial sensitivity of neonatal sepsis: Ten-year experience in one neonatal intensive care unit. J Korean Soc Neonatol. 2009. 16:172–181.16. Chun P, Kong SG, Byun SY, Park SE, Lee HD. Analysis of neonatal sepsis in one neonatal intensive care unit for 6 years. Korean J Pediatr. 2010. 53:495–502.17. Sung JS, Kim DY, Kim SH, Byun HS, Hwang TJ, Choi YY. Analysis of causative microorganisms and choice of antibiotics according to the onset of neonatal sepsis. Korean J Pediatr. 2006. 49:623–629.18. Hwang JH, Choi CW, Chang YS, Choe YH, Park WS, Shin SM, Lee M, Lee SI. The efficacy of clinical strategies to reduce nosocomial sepsis in extremely low birth weight infants. J Korean Med Sci. 2005. 20:177–181.19. Kim BI, Chung HL, Kim YD, Park WS, Shin SM, Lee HJ, Choi JH, Yun CK. Clinical observations on neonatal sepsis. J Korean Pediatr Soc. 1987. 30:130–138.20. Gluck L, Wood HF, Fousek MD. Septicemia of the newborn. Pediatr Clin North Am. 1966. 13:1131–1148.21. Gladstone IM, Ehrenkranz RA, Edberg SC, Baltimore RS. A ten-year review of neonatal sepsis and comparison with the previous fifty-year experience. Pediatr Infect Dis J. 1990. 9:819–825.22. Huang YC, Li CC, Lin TY, Lien RI, Chou YH, Wu JL, Hsueh C. Association of fungal colonization and invasive disease in very low birth weight infants. Pediatr Infect Dis J. 1998. 17:819–822.23. Saiman L, Ludington E, Dawson JD, Saiman L, Ludington E, Dawson JD, Patterson JE, Rangel-Frausto S, Wiblin RT, Blumberg HM, Pfaller M, Rinaldi M, Edwards JE, Wenzel RP, Jarvis W. National Epidemiology of Mycoses Study Group. Risk factors for Candida species colonization of neonatal intensive care unit patients. Pediatr Infect Dis J. 2001. 20:1119–1124.24. El-Masry FA, Neal TJ, Subhedar NV. Risk factors for invasive fungal infection in neonates. Acta Paediatr. 2002. 91:198–202.25. Saiman L, Ludington E, Pfaller M, Rangel-Frausto S, Wiblin RT, Dawson J, Blumberg HM, Patterson JE, Rinaldi M, Edwards JE, Wenzel RP, Jarvis W. Risk factors for candidemia in neonatal intensive care unit patients. The National Epidemiology of Mycosis Survey study group. Pediatr Infect Dis J. 2000. 19:319–324.26. Stoll BJ, Hansen N. Infections in VLBW infants: studies from the NICHD Neonatal Research Network. Semin Perinatol. 2003. 27:293–301.27. Fanaroff AA, Korones SB, Wright LL, Verter J, Poland RL, Bauer CR, Tyson JE, Philips JB 3rd, Edwards W, Lucey JF, Catz CS, Shankaran S, Oh W. For The National Institute of Child Health and Human Development Neonatal Research Network. Incidence, presenting features, risk factors and significance of late onset septicemia in very low birth weight infants. Pediatr Infect Dis J. 1998. 17:593–598.28. Manzoni P, Stolfi I, Pugni L, Decembrino L, Magnani C, Vetrano G, Tridapalli E, Corona G, Giovannozzi C, Farina D, Arisio R, Merletti F, Maule M, Mosca F, Pedicino R, Stronati M, Mostert M, Gomirato G, Italian Task. Italian Task Force for the Study and Prevention of Neonatal Fungal Infections. Italian Society of Neonatology. A multicenter, randomized trial of prophylactic fluconazole in preterm neonates. N Engl J Med. 2007. 356:2483–2495.29. Brecht M, Clerihew L, McGuire W. Prevention and treatment of invasive fungal infection in very low birthweight infants. Arch Dis Child Fetal Neonatal Ed. 2009. 94:F65–F69.30. Van den Hoogen A, Gerards LJ, Verboon-Maciolek MA, Fleer A, Krediet TG. Long-term trends in the epidemiology of neonatal sepsis and antibiotic susceptibility of causative agents. Neonatology. 2010. 97:22–28.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Epidemiology of Early and Late Onset Neonatal Sepsis
- A Case of Neonatal Sepsis with Meningitis due to Gardnerella vaginalis
- The Association between Vitamin D Levels and Neonatal Early-onset Sepsis : A Systematic Review and Meta-analysis
- Predictive factors and initial selection of antibiotics in neonatal sepsis
- Changes in Neonatal Epidemiology during the Last 3 Decades in Korea