J Korean Med Sci.
2009 Oct;24(5):789-794. 10.3346/jkms.2009.24.5.789.
Comparison of Factors Associated with Atypical Symptoms in Younger and Older Patients with Acute Coronary Syndromes
- Affiliations
-
- 1Department of Nursing, College of Medicine, Chosun University, Gwangju, Korea.
- 2The Heart Research Center of Chonnam National University Hospital, Gwangju, Korea. mhjeong@chonnam.ac.kr
- KMID: 1781995
- DOI: http://doi.org/10.3346/jkms.2009.24.5.789
Abstract
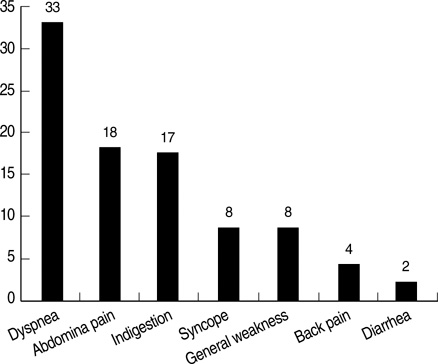
- Patients with acute coronary syndromes (ACS) who are accompanied by atypical symptoms are frequently misdiagnosed and under-treated. This study was conducted to examine and compare the factors associated with atypical symptoms other than chest pain in younger (<70 yr) and older (> or =70 yr) patients with first-time ACS. Data were obtained from the electronic medical records of the patients (n=931) who were newly diagnosed as ACS and hospitalized from 2005 to 2006. The 7.8% (n=49) of the younger patients and 13.4% (n=41) of the older patients were found to have atypical symptoms. Older patients were more likely to complain of indigestion or abdominal discomfort (P=0.019), nausea and/or vomiting (P=0.040), and dyspnea (P<0.001), and less likely to have chest pain (P=0.007) and pains in the arm and shoulder (P=0.018). A logistic regression analysis showed that after adjustment made for the gender and ACS type, diabetes and hyperlipidemia significantly predicted atypical symptoms in the younger patients. In the older patients, the co-morbid conditions such as stroke or chronic obstructive pulmonary disease were positive predictors. Health care providers need to have an increased awareness of possible presence of ACS in younger persons with diabetes and older persons with chronic concomitant diseases when evaluating patients with no chest pain.
Keyword
MeSH Terms
-
Abdominal Pain/etiology
Acute Coronary Syndrome/complications/*diagnosis
Adult
Age Factors
Aged
Aged, 80 and over
Diabetes Mellitus/etiology
Dyspnea/etiology
Female
Humans
Hyperlipidemias/etiology
Male
Middle Aged
Nausea/etiology
Odds Ratio
Predictive Value of Tests
Pulmonary Disease, Chronic Obstructive/etiology
Regression Analysis
Risk Factors
Stroke/etiology
Vomiting/etiology
Figure
Reference
-
1. Brieger D, Eagle KA, Goodman SG, Steg PG, Budaj A, White K, Montalescot G. GRACE Investigators. Acute coronary syndromes without chest pain, an underdiagnosed and undertreated high-risk group: insights from the Global Registry of Acute Coronary Events. Chest. 2004. 126:461–469.2. Canto JG, Shlipak MG, Rogers WJ, Malmgren JA, Frederick PD, Lambrew CT, Ornato JP, Barron HV, Kiefe CI. Prevalence, clinical characteristics, and mortality among patients with myocardial infarction presenting without chest pain. JAMA. 2000. 283:3223–3229.
Article3. Barron HV, Bowlby LJ, Breen T, Rogers WJ, Canto JG, Zhang Y, Tiefenbrunn AJ, Weaver WD. Use of reperfusion therapy for acute myocardial infarction in the United States. Circulation. 1998. 97:1150–1156.
Article4. Milner KA, Funk M, Richards S, Vaccarino V, Krumholz HM. Symptom predictors of acute coronary syndromes in younger and older patients. Nurs Res. 2001. 50:233–241.
Article5. Gregoratos G. Clinical manifestations of acute myocardial infarction in older patients. Am J Geriatr Cardiol. 2001. 10:345–347.
Article6. Patel H, Rosengren A, Ekman I. Symptoms in acute coronary syndromes: Does sex make a difference? Am Heart J. 2004. 148:27–33.
Article7. Arslanian-Engoren C, Patel A, Fang J, Armstrong D, Kline-Rogers E, Duvernoy CS, Eagle KA. Symptoms of men and women presenting with acute coronary syndromes. Am J Cardiol. 2006. 98:1177–1181.
Article8. Ryan CJ, DeVon HA, Horne R, King KB, Milner K, Moser DK, Quinn JR, Rosenfeld A, Hwang SY, Zerwic JJ. Symptom clusters in acute myocardial infarction: a secondary data analysis. Nurs Res. 2007. 56:72–81.9. Milner KA, Funk M, Arnold A, Vaccarino V. Typical symptoms are predictive of acute coronary syndromes in women. Am Heart J. 2002. 143:283–288.
Article10. Then KL, Rankin JA, Fofonoff DA. Atypical presentation of acute myocardial infarction in 3 age groups. Heart Lung. 2001. 30:285–293.
Article11. Goldberg RJ, Yarzebski J, Lessard D, Gore JM. Decade-long trends and factors associated with time to hospital presentation in patients with acute myocardial infarction: The Worcester Heart Attack Study. Arch Intern Med. 2000. 160:3217–3223.12. Han JH, Lindsell CJ, Hornung RW, Lewis T, Storrow AB, Hoekstra JW, Hollander JE, Miller CD, Peacock WF, Pollack CV, Gibler WB. Emergency medicine cardiac research and education group internet tracking registry for acute coronary syndromes investigators. The elder patient with suspected acute coronary syndromes in the emergency department. Acad Emerg Med. 2007. 14:732–739.
Article13. Stephen SA, Darney BG, Rosenfeld AG. Symptoms of acute coronary syndrome in women with diabetes: an integrative review of the literature. Heart Lung. 2008. 37:179–189.
Article14. Franklin K, Goldberg RJ, Spencer F, Klein W, Budaj A, Brieger D, Marre M, Steg PG, Gowda N, Gore JM. GRACE investigators. Implications of diabetes in patients with acute coronary syndromes. Arch Intern Med. 2004. 164:1457–1463.15. Chun BY, Dobson AJ, Heller RF. The impact of diabetes on survival among patients with first myocardial infarction. Diabetes Care. 1997. 20:704–708.
Article16. Lowel H, Koenig W, Engel S, Horman A, Keil U. The impact of diabetes mellitus on survival after myocardial infarction: can it be modified by drug treatment? Results of a population-based myocardial infarction register follow-up study. Diabetologica. 2000. 43:218–226.17. Bakhai A, Collinson J, Flather MD, de Arenaza DP, Shibata MC, Wang D, Adgey JA. KAA Fox for the PRAIS-UK Investigators. Diabetic patients with acute coronary syndromes in the UK: high risk and under treated. Results from the prospective registry of acute ischaemic syndromes in the UK (PRAIS-UK). Int J Cardiol. 2005. 100:79–84.
Article18. Herlitz J, Karlson BW, Lindqvist J, Sjölin M. Important factors for the 10-year mortality rate in patients with acute chest pain or other symptoms consistent with acute myocardial infarction with particular emphasis on the influence of age. Am Heart J. 2001. 142:624–632.
Article19. DeVon HA, Ryan CJ. Symptoms across the continuum of acute coronary syndromes: differences between women and men. Am J Crit Care. 2008. 17:14–25.
Article20. Lingman M, Herlitz J, Bergfeldt L, Karlsson T, Caidahl K, Hartford M. Acute coronary syndromes-the prognostic impact of hypertension, diabetes and its combination on long-term outcome. Int J Cardiol. 2009. 137:29–36.21. Mak KH, Moliterno DJ, Granger CB, Miller DP, White HD, Wilcox RG, Califf RM, Topol EJ. For the global utilization of streptokinase and tissue plasminogen activator for occluded coronary arteries (GUSTO)-1 investigators. Influence of diabetes mellitus on clinical outcome in the thrombolytic era of acute myocardial infarction. J Am Coll Cardiol. 1997. 30:171–179.22. Ruston A, Clayton J. Women's interpretation of cardiac symptoms at the time of their cardiac event: The effect of co-occurring illness. Eur J Cardio Nurs. 2007. 6:321–328.
Article23. Dracup K, McKinley S, Riegel B, Mieschke H, Doering LV, Moser DK. A nursing intervention to reduce prehospital delay in acute coronary syndrome: a randomized clinical trial. J Cardiovasc Nurs. 2006. 21:186–193.24. Tullmann DF, Haugh KH, Dracup KA, Bourguignon C. A randomized controlled trial to reduce delay in older adults seeking help for symptoms of acute myocardial infarction. Res Nurs Health. 2007. 30:485–497.
Article25. Buckley T, McKinley S, Gallagher R, Dracup K, Moser DK, Aitken LM. The effect of education and counseling on knowledge, attitudes and beliefs about responses to acute myocardial infarction symptoms. Eur J Cardiovasc Nurs. 2007. 6:105–111.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Comparison of Clinical Manifestations and Treatment-Seeking Behavior in Younger and Older Patients with First-time Acute Coronary Syndrome
- Antithrombotic Therapy for Elderly Patients with Acute Coronary Syndrome
- Three cases of atypical Kawasaki disease with coronary aneurysm
- Does arterial hypotension due to cardiogenic shock in older patients lead to functional oliguria or to acute renal failure?
- Atypical Symptom Cluster Predicts a Higher Mortality in Patients With First-Time Acute Myocardial Infarction