J Korean Med Sci.
2005 Oct;20(5):904-907. 10.3346/jkms.2005.20.5.904.
Lymphangiomyomatosis Arising in the Pelvic Cavity: A Case Report
- Affiliations
-
- 1Department of Pathology, Chungnam National University School of Medicine, Daejeon, Korea. kssuh@cnu.ac.kr
- KMID: 1781783
- DOI: http://doi.org/10.3346/jkms.2005.20.5.904
Abstract
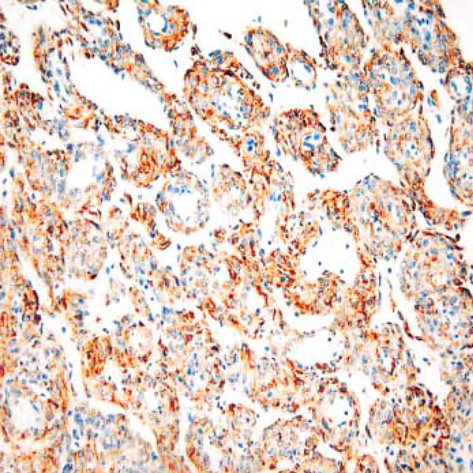
- Lymphangioleiomyomatosis (LAM) is a rare disease usually occurring in young women of child-bearing age. It is characterized by a distinctive proliferation of lymphatic smooth muscle cells, especially occurring in the pulmonary parenchyme. The majority of primary LAM occurs in the lung, but there are a few reports of extrapulmonary cases. We report a case of a 21-yr-old female who first complained of low abdominal pain and was referred from a local clinic with the impression of an ovarian cyst. Gynecologic ultrasonography revealed a large posterior pelvic mass with an irregular echogenicity measuring 9.7x4.2 cm in size. Pelviscopy showed a large, thin walled, partly cystic, pelvic mass. The mass was partly removed. Microscopically, the mass was characterized by a haphazard proliferation of smooth muscle cells arranged in fascicular, trabecular, and papillary patterns around a ramifying network of endothelium-lined spaces. The cells were plump or epithelioid with abundant eosinophilic cytoplasm and showed a positive reaction for both alpha-smooth muscle actin and HMB-45 antigen. Surgical and pathological findings were consistent with pelvic retroperitoneal LAM. Despite the numerous treatment attempts, the patient suffered from intractable chylous ascites and developed pulmonary LAM and died due to severe respiratory distress.
MeSH Terms
Figure
Reference
-
1. Zamboni G, Pea M, Martignoni G, Zancanaro C, Faccioli G, Gilioli E, Pederzoli P, Bonetti F. Clear cell "sugar" tumor of the pancreas. A novel member of the family of lesions characterized by the presence of perivascular epithelioid cells. Am J Surg Pathol. 1996. 20:722–730.2. Chu SC, Horiba K, Usuki J, Avila NA, Chen CC, Travis WD, Ferrans VJ, Moss J. Comprehensive evaluation of 35 patients with lymphangioleiomyomatosis (LAM). Chest. 1999. 115:1041–1052.3. Matsui K, Tatsuguchi A, Valencia J, Yu Z, Bechtle J, Beasley MB, Avila N, Travis WD, Moss J, Ferrans VJ. Extrapulmonary lymphangioleiomyomatosis (LAM): clinicopathologic features in 22 cases. Hum Pathol. 2000. 31:1242–1248.
Article4. Chan JK, Tsang WY, Pau MY, Tang MC, Pang SW, Fletcher CD. Lymphangiomyomatosis and angiomyolipoma: closely related entities characterized by hamartomatous proliferation of HMB-45 positive smooth muscle. Histopathology. 1993. 22:445–455.5. National Heart, Lung, and Blood Institute. NHLBI Workshop Summary. Report of workshop on lymphangioleiomyomatosis. Am J Respir Crit Care Med. 1999. 159:679–683.6. Jaiswal VR, Baird J, Fleming J, Miller DS, Sharma S, Molberg K. Localized retroperitoneal lymphangioleiomyomatosis mimicking malignancy. Arch Pathol Lab Med. 2003. 127:879–882.
Article7. Kim GY, Lee J, Park YK, Kim YW, Park JH, Yang MH. Pulmonary lymphangioleiomyomatosis and micronodular pneumocyte hyperplasia associated with tuberous sclerosis: A case report. Korean J Pathol. 2002. 36:51–54.8. Mo EK, Jung MP, Yoo CG, Kim YW, Han SK, Im JG, Seo JW, Lee SS, Shim YS, Kim KY, Han YC. Lymphangioleiomyomatosis in Korea. Tuberc Respir Dis. 1993. 40:519–531.
Article9. Kwon T, Chung NE. Pulmonary lymphangioleiomyomatosis associated with a fatal pneumothorax: an autopsy case report. Korean J Leg Med. 2000. 24:61–65.10. Hancock E, Tomkins S, Sampson J, Osborne J. Lymphangioleiomyomatosis and tuberous sclerosis. Respir Med. 2002. 96:7–13.
Article11. Moss J, Avila NA, Barnes PM, Litzenberger RA, Bechtle J, Brooks PG, Hedin CJ, Hunsberger S, Kristof AS. Prevalence and clinical characteristics of lymphangioleiomyomatosis (LAM) in patients with tuberous sclerosis complex. Am J Respir Crit Care Med. 2001. 164:669–671.
Article12. Carsillo T, Astrinidis A, Henske EP. Mutations in the tuberous sclerosis complex gene TSC2 are a cause of sporadic pulmonary lymphangioleiomyomatosis. Proc Natl Acad Sci USA. 2000. 97:6085–6090.
Article13. Strizheva GD, Carsillo T, Kruger WD, Sullivan EJ, Ryu JH, Henske EP. The spectrum of mutations in TSC1 and TSC2 in women with tuberous sclerosis and lymphangiomyomatosis. Am J Resp Crit Care Med. 2001. 163:253–258.14. Matsui K, Takeda K, Yu ZX, Valencia J, Travis WD, Moss J, Ferrans VJ. Downregulation of estrogen and progesterone receptors in the abnormal smooth muscle cells in pulmonary lymphangioleiomyomatosis following therapy. An immunohistochemical study. Am J Respir Crit Care Med. 2000. 161:1002–1009.15. Logginidou H, Ao X, Russo I, Henske EP. Frequent estrogen and progesterone receptor immunoreactivity in renal angiomyolipomas from women with pulmonary lymphangioleiomyomatosis. Chest. 2000. 117:25–30.
Article16. Sullivan EJ. Lymphangioleiomyomatosis: a review. Chest. 1998. 114:1689–1703.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Ganglioneuroma in Pelvic Cavity
- Lymphangiomyomatosis discovered by massive hemoptysis during general anesthesia: A case report
- A Case of Localized fibrous tumor of Pelvic Cavity
- An Inguinal Endometriosis without Any Other Pelvic Endometriosis Mimicking Direct Inguinal Hernia: A Case Report
- A case of myxoid malignant fibrous histiocytoma in the pelvic cavity